Medication Interactions: What You Need to Know Before Taking Pills Together
When you take more than one medication, you’re not just adding effects—you’re creating a new chemical environment inside your body. Medication interactions, happen when two or more drugs react in ways that change how they work, increase side effects, or cause unexpected harm. Also known as drug interactions, they’re one of the most underreported causes of hospital visits and preventable health crises. This isn’t just about prescription pills. It includes over-the-counter painkillers, supplements like magnesium hydroxide or garden cress extracts, and even herbal remedies. A simple combo like ibuprofen and a blood thinner might seem harmless, but it can spike your risk of internal bleeding. Or take doxylamine—a common sleep aid—mixed with other sedatives. It doesn’t just make you drowsy; it can slow your breathing to dangerous levels.
These reactions aren’t random. They follow patterns. Some drugs slow down how your liver breaks down others, causing buildup. Others compete for the same receptors in your brain or gut, canceling each other out. Compounded medications, custom formulas made for individual needs, often carry hidden interaction risks because they’re not tested in large populations. Even generics, which are legally required to match brand-name drugs in strength, can behave differently when mixed with other substances due to inactive ingredients. And if you’re using something like modified-release formulations, drugs designed to release slowly over hours, alcohol or certain foods can break that system open, flooding your system all at once. That’s why a pill that’s safe alone becomes risky in combination.
It’s not just about what you’re taking—it’s about who you are. Age, liver function, kidney health, and even your diet change how these reactions play out. Someone on a low-sodium diet might react differently to a diuretic than someone who eats salty snacks daily. A person with myasthenia gravis might have a heightened sensitivity to muscle-relaxing drugs. And if you’re using something like hydroxyzine for IBS or celecoxib for joint pain, those drugs don’t just sit there—they talk to your brain, your gut, your heart. One study found that nearly 40% of adults over 65 take at least five medications daily. That’s a recipe for unnoticed clashes.
You don’t need to memorize every possible combo. But you do need to know how to ask the right questions. When your doctor writes a new script, ask: "Could this interact with anything else I’m taking?" Bring a list—not just prescriptions, but vitamins, teas, CBD oils, and supplements. Pharmacists are trained to catch these. They see the patterns you miss. And if you’ve ever had a rash after starting a new pill, or felt dizzy when you added a supplement, that’s not coincidence—it’s a signal.
Below, you’ll find real-world examples of how these interactions show up in everyday use—from how alcohol ruins extended-release pills, to why mixing certain painkillers with antidepressants can trigger serotonin syndrome. You’ll see what happens when people assume "natural" means safe, and how even something as simple as magnesium hydroxide can interfere with antibiotics. These aren’t theory pieces. They’re stories from people who learned the hard way—and the clear, practical advice that can keep you from making the same mistake.
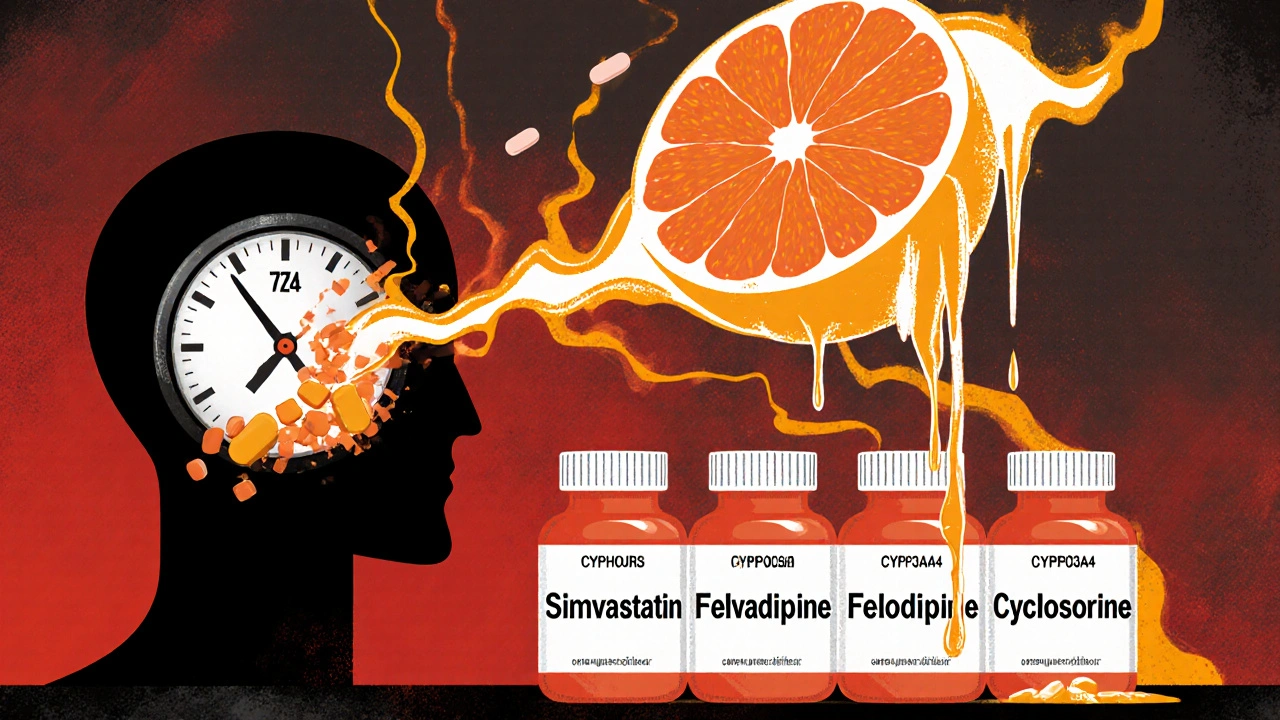
Grapefruit Juice Interactions: Why Some Medications Are Dangerous When Mixed
13 Comments
Grapefruit juice can dangerously increase levels of certain medications by blocking enzymes that break them down. Over 85 drugs interact with it - including statins, blood pressure meds, and immunosuppressants. Avoid it completely if you're on one.
Read More