One glass of grapefruit juice in the morning might seem like a healthy start - but if you're taking certain medications, it could be life-threatening. This isn't a myth or a warning from an overcautious doctor. It’s a well-documented, clinically proven danger that affects tens of thousands of people every year. The problem isn’t the juice itself. It’s what happens when grapefruit meets your pills.
How Grapefruit Juice Changes How Your Body Handles Medication
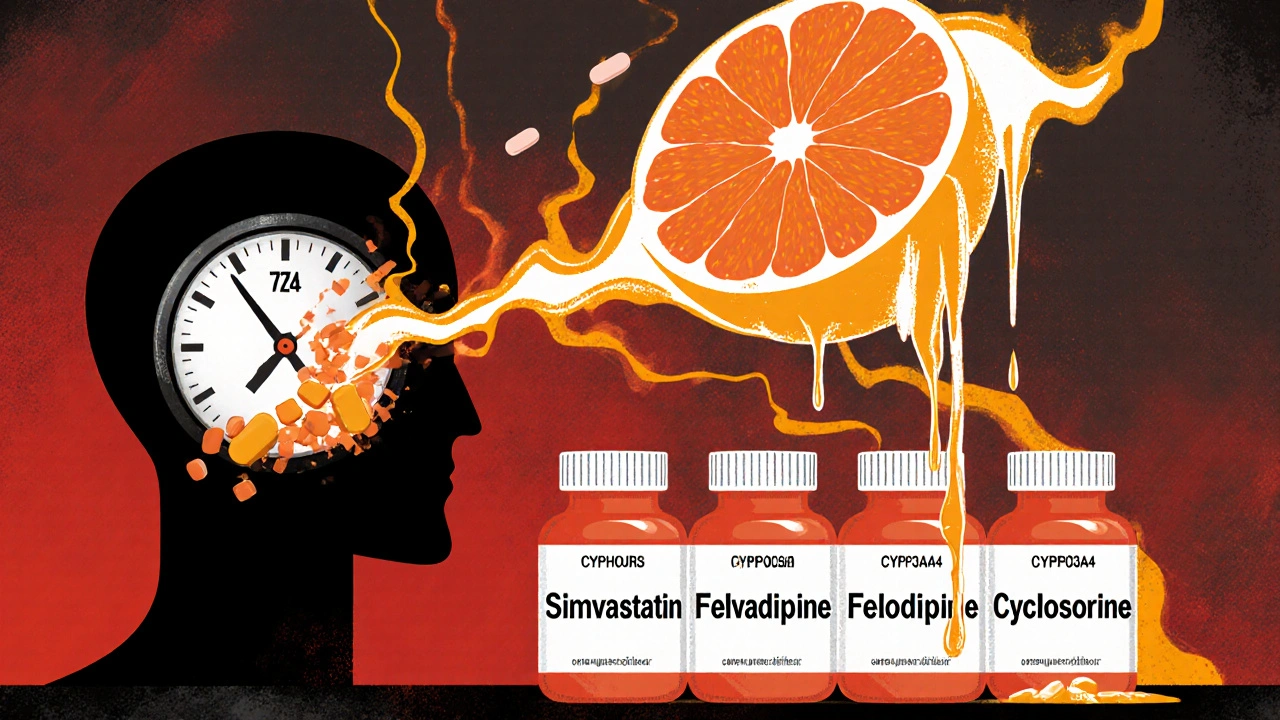
Most drugs you take are broken down by enzymes in your gut before they ever reach your bloodstream. One key enzyme, called CYP3A4, acts like a gatekeeper - it chops up many medications so only a safe amount enters your system. Grapefruit juice doesn’t just slow this process down. It shuts it off - permanently - for a few days.
The culprits are chemicals in grapefruit called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds bind to CYP3A4 enzymes in your intestinal wall and destroy them. Your body can’t just rebuild them overnight. It takes about three days for new enzymes to replace what’s been lost. That means if you drink grapefruit juice on Monday, your body is still vulnerable on Wednesday - even if you didn’t drink any on Tuesday.
This isn’t a small change. For some drugs, grapefruit juice can increase the amount in your blood by 300% to 800%. That’s not a little extra. That’s enough to push a safe dose into the dangerous zone.
Which Medications Are Most at Risk?
Not all drugs are affected the same way. Some aren’t touched at all. Others? They’re in serious danger.
Statins - the cholesterol-lowering drugs - show the clearest pattern. Simvastatin and lovastatin are extremely sensitive. Just one glass of grapefruit juice can cause simvastatin levels to spike by 330%. That raises your risk of rhabdomyolysis - a condition where muscle tissue breaks down, releasing toxins that can wreck your kidneys. Atorvastatin is also risky, but pravastatin, rosuvastatin, and fluvastatin? They’re safe. Why? Because they’re processed by different enzymes.
Calcium channel blockers like felodipine and nifedipine are next on the list. Felodipine’s blood levels can jump up to 8 times higher after grapefruit juice. That can cause dangerously low blood pressure, dizziness, fainting, or even heart rhythm problems. Amlodipine, however, is barely affected.
Benzodiazepines like midazolam (used for sedation) can become much stronger - up to 515% more potent. That means you could end up overly sedated, with slowed breathing. Triazolam is less affected, but still risky.
Immunosuppressants like cyclosporine and tacrolimus are especially dangerous. These drugs have narrow safety margins - the difference between the right dose and a toxic one is tiny. Grapefruit juice can push levels into the toxic range, increasing the risk of kidney damage or infection.
Antiarrhythmics like amiodarone and some antidepressants like sertraline also interact. Even some antibiotics and erectile dysfunction drugs (like sildenafil) can be affected.
Here’s what you need to know: if your medication label says "avoid grapefruit," it’s not a suggestion. It’s a warning.
It’s Not Just Juice - It’s Everything Grapefruit
You might think, "I don’t drink juice, I eat the fruit." That doesn’t help. The same chemicals are in the flesh, the peel, even the pulp. Fresh fruit, frozen concentrate, canned segments - they all contain enough furanocoumarins to cause problems.
Even white grapefruit is worse than pink. White varieties have 20-50% more of the dangerous compounds. And it doesn’t matter if it’s organic, fresh-squeezed, or store-bought. The interaction isn’t about sugar or additives. It’s about chemistry.
And it’s not just grapefruit. Seville oranges (used in marmalade) and pomelos contain the same chemicals. Regular oranges, tangerines, and clementines? Safe. No interaction. You can drink orange juice without worry.

Why Do Some People Get Hit Harder Than Others?
Not everyone reacts the same way. One person might drink grapefruit juice with their statin and feel fine. Another might end up in the hospital. Why?
It comes down to your genetics and your gut. Some people naturally have more CYP3A4 enzymes in their intestines. When grapefruit knocks those out, the drop is bigger - so the drug level spikes higher. Studies show this difference can range from zero to eightfold increase in blood levels, even with the same amount of juice.
There’s also a genetic marker - CYP3A4*22 - that makes some people more vulnerable. This variant is rare, but if you have it, grapefruit juice could be extra dangerous. Right now, doctors don’t routinely test for it, but research is moving in that direction.
Age matters too. Older adults are at higher risk. Why? They’re more likely to be on multiple medications. One study found that 42% of adults over 65 take five or more drugs - and many of those are affected by grapefruit. Add to that slower metabolism and reduced kidney function, and the risk compounds.
What Should You Do If You’re on Medication?
Step one: Check your prescription label. If it says "avoid grapefruit," do it. No exceptions.
Step two: Ask your pharmacist. Not your doctor. Pharmacists are the drug experts. They see every medication you’re on and know which ones interact. If you’ve filled a prescription in the last year, they’ve seen it. Ask them: "Is there anything in my medications that reacts with grapefruit?"
Step three: If you’re taking a high-risk drug, avoid grapefruit entirely for at least 72 hours before and during treatment. Don’t try to time it. Don’t think, "I’ll have it at night, not in the morning." The enzyme damage lasts for days. Timing doesn’t fix it.
Step four: If you’re on a drug like simvastatin or felodipine and you’ve been drinking grapefruit juice, talk to your doctor about switching to a safer alternative. Pravastatin, rosuvastatin, or amlodipine are often just as effective - without the risk.

Why Don’t More People Know About This?
It’s shocking, but true: only 37% of pharmacists consistently warn patients about grapefruit interactions. And only 28% of patients can correctly name which of their meds are affected - even after being told.
Doctors don’t always know. Pharmacists are busy. Labels are small. Patients assume if it’s natural, it’s safe. That’s the dangerous myth.
And here’s the kicker: the FDA now requires grapefruit warnings on 21 high-risk medications. But 85 drugs total are known to interact. That means nearly two-thirds of risky medications don’t even have a warning on the label.
That’s why you can’t rely on labels alone. You have to ask.
What’s Being Done to Fix This?
Things are slowly changing. Electronic health records now have over 128 built-in alerts for grapefruit interactions. Drug interaction software flags this problem in 18% of all food-drug cases. Pharmaceutical companies are reformulating drugs - like extended-release felodipine - to reduce the risk.
Researchers are even working on CRISPR-edited grapefruit that lack furanocoumarins. It’s still in trials, but if it works, you might one day enjoy grapefruit without worry.
For now, though, the safest advice remains the same: if your medication is on the list, skip it. No compromise.
What If You’ve Already Had a Glass?
If you drank grapefruit juice and just realized your medication is risky, don’t panic. But don’t ignore it either.
Stop drinking grapefruit juice immediately. Monitor yourself for symptoms: unexplained muscle pain, weakness, dark urine, dizziness, fainting, irregular heartbeat, or extreme fatigue. These could be signs of serious side effects.
Contact your pharmacist or doctor. Tell them what you took, when, and how much grapefruit you had. They can advise whether you need to be checked.
Don’t wait for symptoms. Some reactions take hours. Others take days. Better safe than sorry.
And remember - this isn’t about being perfect. It’s about being informed. One glass can change everything. But knowing the risk? That’s power.
Can I have orange juice instead of grapefruit juice if I’m on medication?
Yes. Regular orange juice, tangerines, and clementines do not contain furanocoumarins and do not interfere with medications. You can safely drink them while on most drugs. But avoid Seville oranges and pomelos - they act just like grapefruit.
How long does grapefruit juice affect my medication?
The enzyme-blocking effect lasts about 72 hours - three full days. Even if you drink grapefruit juice at night, it can still affect your morning pill. That’s why simply spacing them out doesn’t work. You need to avoid it completely for the duration of your treatment.
Does it matter if I eat the fruit or drink the juice?
No. The active chemicals are in the flesh, peel, and pulp - not just the juice. Whether you eat a whole grapefruit, drink freshly squeezed juice, or eat canned segments, you’re getting the same interaction risk. All forms are equally dangerous with affected medications.
Are there any medications that grapefruit juice makes less effective?
Yes, but it’s rare. Grapefruit juice can reduce absorption of some drugs like fexofenadine (Allegra) by blocking OATP transporters in the gut. It can also lower levels of theophylline and itraconazole, though the reasons aren’t fully understood. The bigger risk is drugs becoming too strong - not too weak.
Is it safe to have grapefruit juice once in a while if I’m on a low dose?
No. Even small amounts of grapefruit juice can trigger a major interaction. A single 200mL glass (about 6.8 fl oz) is enough to block intestinal enzymes. Dose doesn’t matter - the mechanism is all-or-nothing. If your drug is on the high-risk list, avoid it completely.
Why don’t all drug labels warn about grapefruit juice?
The FDA requires warnings on 21 high-risk medications, but there are 85 known interactions. Many drugs still don’t carry warnings because manufacturers haven’t updated labels, or the interaction was discovered after approval. Don’t assume no label means no risk. Always ask your pharmacist.
Can I switch to a different medication to avoid grapefruit juice?
Yes, often. For example, if you’re on simvastatin, your doctor can switch you to rosuvastatin or pravastatin - both work just as well for cholesterol and don’t interact with grapefruit. Same with calcium channel blockers: amlodipine is a safe alternative to felodipine. Always ask your doctor if a safer option exists.
Comments
Prem Hungry November 18, 2025 at 19:17
bro i took simvastatin for like 6 months and drank grapefruit juice every morning… nothin happened. maybe my body just don’t care. 🤷♂️
Leslie Douglas-Churchwell November 20, 2025 at 01:44
THIS IS A PHARMA-CONTROLLED DISINFORMATION CAMPAIGN. 🍊💥 The FDA only mandates warnings on 21 drugs because they’re in bed with Big Pharma. The real danger? The CYP3A4 enzyme suppression is a *deliberate* metabolic bottleneck engineered to keep you dependent on synthetic compounds. Meanwhile, nature’s own furanocoumarins are the *true* detox pathway - but they’re being demonized to sell you pravastatin at 3x the price. 🌱💸 #GrapefruitIsTheResistance
shubham seth November 21, 2025 at 16:09
Let’s be real - grapefruit juice is basically a biological nuke for your liver enzymes. It’s like throwing a Molotov cocktail into your gut’s drug-processing factory. Simvastatin + grapefruit? That’s not a side effect, that’s a full-on biochemical coup. And the worst part? You don’t even feel it until your muscles start dissolving into your urine. 😬
Kathryn Ware November 23, 2025 at 00:33
Just wanted to say thank you for this incredibly thorough breakdown - I’m a nurse and I’ve seen *so* many patients get hospitalized because they thought ‘natural’ meant ‘safe.’ 🙏 I always tell my patients: if your med has a grapefruit warning, treat it like a live grenade. And yes - orange juice is totally fine! 🍊➡️🍊 (just not Seville or pomelo!!) I even made a little handout for my clinic: ‘Grapefruit = No. Orange = Yay. Pomelo = Nope. Mandarin = Chill.’ 😊
Tarryne Rolle November 24, 2025 at 11:22
What if the real danger isn’t the grapefruit… but the assumption that we can control biology with pills? We take synthetic compounds, then get mad when nature fights back. The body isn’t a machine. It’s a symphony - and grapefruit isn’t the villain. We are, for thinking we can outsmart evolution with a prescription.
Kyle Swatt November 25, 2025 at 16:20
People act like this is some secret scandal but it’s been in the medical journals since the 90s. I’ve got my dad on felodipine and he used to guzzle grapefruit juice like it was water. Told him flat out - if you want to drop dead on the couch watching football, fine. But don’t make me clean up your mess. He switched to amlodipine. Still alive. Still pissed at me. Worth it.
Deb McLachlin November 26, 2025 at 21:30
Thank you for including the genetic component - the CYP3A4*22 variant is rarely discussed in patient education materials. I’m curious if any recent studies have explored population-level prevalence of this variant in South Asian populations, given the high incidence of statin use in India. The pharmacogenomic implications could be significant for public health policy.
saurabh lamba November 27, 2025 at 04:18
so like… if i just eat one slice once a year… is that cool? 🍊
Kiran Mandavkar November 27, 2025 at 08:01
Typical Western medical arrogance. You think a single enzyme is the gatekeeper of health? You ignore Ayurveda, Traditional Chinese Medicine, and millennia of herbal wisdom. Grapefruit isn’t dangerous - your reliance on synthetic drugs is. The body knows how to heal. You just need to stop poisoning it with pills and start listening.
Eric Healy November 27, 2025 at 15:39
you guys are missing the point. if you're on a statin and you drink grapefruit juice you're not just risking rhabdo you're basically asking for a one way ticket to the ICU. i've seen it. its not pretty. and no its not just for simva. lovastatin is the worst but even atorva can go sideways. just stop. please. for the love of god stop.
Shannon Hale November 27, 2025 at 19:11
MY BEST FRIEND DIED FROM THIS. 🕯️ She took simvastatin. Ate half a grapefruit. Thought it was ‘healthy.’ She woke up with muscle pain, went to urgent care, they said ‘muscle strain.’ Three days later she was in the ER with kidney failure. They couldn’t save her. This isn’t a ‘warning.’ It’s a death sentence if you ignore it. STOP TRUSTING YOUR GUT. TRUST THE LABEL. SHE WAS 42.
Holli Yancey November 28, 2025 at 18:32
I really appreciate how this post doesn’t just list drugs but explains why the interaction happens. It’s easy to say ‘avoid grapefruit’ but understanding the enzyme destruction makes it click. I used to think timing it would help - like drinking juice at night - but now I get why it’s a 3-day window. I’ll be sharing this with my mom who’s on cyclosporine.
Gordon Mcdonough November 29, 2025 at 22:44
AMERICA IS GETTING SOFT. Back in my day we took our meds and our grapefruit and we didn’t whine about it. Now you need a PhD to drink juice? This is why we lost the war on drugs - because people think a fruit is a weapon. Just take your pills. Eat your fruit. Life’s short. Live a little. 🍊💊 #StopTheFear