Understanding Eosinophilic Esophagitis and Budesonide
Eosinophilic esophagitis (EoE) is a chronic immune-mediated disorder affecting the esophagus, leading to inflammation, difficulty swallowing, and other symptoms. Budesonide is a corticosteroid medication that has shown promise in treating EoE. In this section, we will explore what EoE is, how it affects those who suffer from it, and the role budesonide plays in its treatment. By understanding the relationship between EoE and budesonide, we can better appreciate the importance of proper treatment and management of this condition.
Diagnosing Eosinophilic Esophagitis
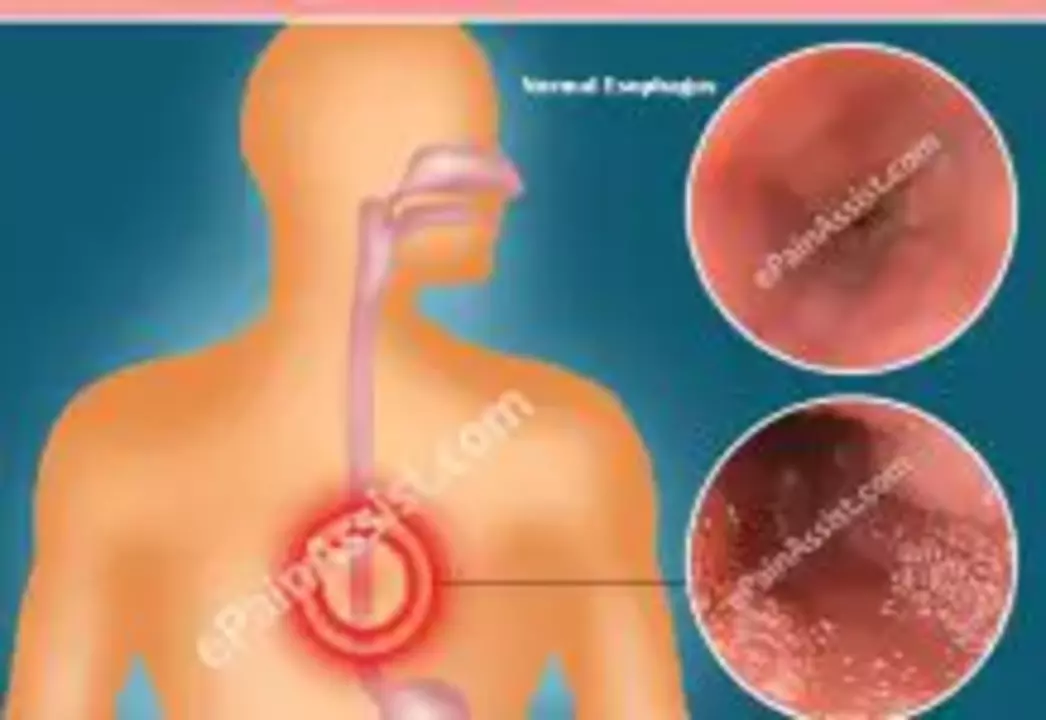
Diagnosing EoE can be a challenging process, as its symptoms often overlap with other gastrointestinal disorders. In order to accurately diagnose EoE, a combination of clinical symptoms, endoscopic findings, and histological evidence of eosinophilic infiltration in the esophageal tissue is required. This typically involves undergoing an upper endoscopy, during which a small tissue sample is taken for examination under a microscope. Once a diagnosis has been made, a treatment plan can be developed to help manage the symptoms and inflammation associated with EoE.
Budesonide: An Effective Treatment Option
Budesonide has emerged as a popular and effective treatment option for EoE due to its potent anti-inflammatory properties. It works by reducing the number of eosinophils in the esophagus, which in turn can help alleviate the symptoms and discomfort associated with the condition. Budesonide is available in various forms, including oral tablets, inhalation, and as a liquid suspension that can be swallowed. The choice of formulation will depend on the individual patient's needs and preferences, as well as the advice of their healthcare provider.
How to Properly Use Budesonide for EoE
When using budesonide to treat EoE, it is crucial to follow the prescribed dosage and administration instructions provided by your healthcare provider. This may include specific instructions on how to take the medication, such as whether it should be taken with food or on an empty stomach. Additionally, it is essential to adhere to the prescribed treatment duration, as stopping the medication too soon may result in a relapse of symptoms. If you experience any side effects or concerns while using budesonide, be sure to discuss them with your healthcare provider to ensure the best possible outcome for your treatment.
Monitoring Progress and Adjusting Treatment
Regular monitoring is an important aspect of managing EoE and assessing the effectiveness of budesonide treatment. This may involve periodic endoscopies to evaluate the esophageal tissue and ensure that inflammation and eosinophil levels are improving. If the desired results are not achieved, your healthcare provider may need to adjust the treatment plan, which could involve changes to the dosage or formulation of budesonide, or even the addition of other medications or therapies. It is important to maintain open communication with your healthcare team throughout the treatment process to ensure the best possible outcome.
Living with Eosinophilic Esophagitis: Tips for Managing Symptoms
While budesonide can be an effective treatment for managing the inflammation and symptoms of EoE, it is also essential to incorporate lifestyle modifications and self-care strategies to help improve your overall quality of life. This may include dietary changes, such as eliminating common food triggers or working with a registered dietitian to develop a personalized meal plan. Additionally, practicing stress management techniques and staying informed about your condition can help you feel more in control and better equipped to cope with the challenges of living with EoE.
Comments
AnGeL Zamorano Orozco May 14, 2023 at 13:42
Listen up, because the battle against eosinophilic esophagitis is nothing short of a warzone and budesonide is the *only* weapon that can possibly hold the line. This corticosteroid swoops in like a rogue hero, slashing eosinophil counts with a ferocity that would make a tiger jealous. You take it as a liquid suspension, and if you dare forget a dose, the inflammation rebounds like a boomerang, striking harder than before. The side effects? Yeah, they’re there, but who gives a damn when you’re finally able to swallow a sandwich without pain? Studies show that a two‑month regimen can bring histology down to near‑normal, and that’s just the beginning of the saga. Patients who stop too early often experience a relapse that feels like the condition is mocking them. So, you better stick to the prescribed schedule, even if your calendar feels like a prison. The dosage is carefully calibrated; too much can cause systemic effects, too little and you’ll be stuck in a loop of endless endoscopies. And let’s not ignore the fact that many doctors still hesitate to prescribe it, fearing the hype over steroids. The truth? Budesonide’s local action in the esophagus minimizes systemic absorption, making it a relatively safe bet. If you’re thinking about combining it with dietary changes, go ahead-just don’t expect miracles without the drug. The real hero here is the patient’s discipline, not some mystical cure. Remember, the esophagus is a delicate tube; you can’t treat it like a rubber band you just stretch and forget. So keep that medication handy, follow up with your gastroenterologist, and pray the universe grants you a smooth passage through the foods you love. And if you ever feel the burning sensation creep back, that’s a sign you missed a dose-get your act together and stay on track. The battle is tough, the stakes are high, but with budesonide you’ve got a fighting chance, even if it feels like you’re walking a tightrope over a pit of fire.
Cynthia Petersen May 14, 2023 at 19:15
Oh great, another "miracle" drug that apparently does everything except your taxes. Let’s be real: budesonide does cut down eosinophil counts, but you still need to watch your diet like a hawk. It’s not a free pass to binge on spicy tacos anymore. Also, the risk of oral candidiasis is like that annoying neighbor who never leaves. You’ll still have to deal with the occasional throat irritation-thanks, steroids! And yes, regular endoscopies are a must, because who doesn’t love another invasive procedure? Bottom line, it’s helpful, but don’t expect it to turn you into a superhero overnight.
Marcia Hayes May 15, 2023 at 00:49
Totally hear you! I’ve been on the suspension for a few months and the swallowing pain has seriously dropped. Just remember to keep the bottle refrigerated.
Danielle de Oliveira Rosa May 15, 2023 at 06:22
Considering the immunological nature of eosinophilic esophagitis, budesonide’s localized anti‑inflammatory action offers a compelling therapeutic avenue. By targeting the esophageal mucosa directly, systemic exposure is minimized, which aligns with the principle of precision medicine. Moreover, the reduction in eosinophilic infiltration often correlates with improved histopathological outcomes, a fact supported by multiple peer‑reviewed studies. Patients should, however, be counseled about the importance of adherence to prevent relapse. Ultimately, integrating pharmacologic intervention with lifestyle modifications yields the most sustainable remission.
Tarun Rajput May 15, 2023 at 11:55
Indeed, the elegance of a locally acting glucocorticoid such as budesonide lies in its capacity to modulate the inflammatory cascade without invoking the systemic sequelae typically associated with oral corticosteroids. The physician’s role, in this context, is to tailor the dosage regimen-often commencing with a 1 mg twice‑daily protocol-while remaining vigilant for adverse events like adrenal suppression, albeit rare. It is prudent to schedule follow‑up endoscopic assessments at intervals of three to six months to objectively gauge histologic remission, thereby informing potential dose tapering strategies. Additionally, interdisciplinary collaboration with dietitians can enhance therapeutic outcomes, as elimination diets synergistically reduce antigenic stimulation. One must also acknowledge the pharmacokinetic nuance that budesonide’s high first‑pass metabolism confers a favorable safety margin, making it an optimal choice for long‑term management. In summary, when wielded judiciously, budesonide embodies a paradigm of targeted therapy, marrying efficacy with safety, provided that clinicians and patients alike remain committed to rigorous monitoring and adherence.
Joe Evans May 15, 2023 at 18:52
Great info! 😊
Colin Boyd May 16, 2023 at 00:25
While many hail budesonide as a panacea for EoE, let us not forget that steroid resistance can emerge, even in the esophageal milieu. One should consider adjunctive therapies rather than relying solely on a single agent.
John Petter May 16, 2023 at 05:59
Reading about budesonide feels like perusing a textbook written for gastroenterology elites. It’s impressive, yet I wonder why the layperson never sees this in plain language.
Annie Tian May 16, 2023 at 11:32
The data are indeed compelling; however, it is essential to maintain realistic expectations. Budesonide can significantly reduce inflammation, but it does not guarantee a cure. Continuous monitoring and patient education remain paramount; without them, even the best pharmacologic regimen may falter. Moreover, integrating dietary strategies can augment therapeutic success. In practice, a multidisciplinary approach yields the most favorable outcomes.
April Knof May 16, 2023 at 17:05
From a cultural standpoint, the acceptance of steroid therapy varies across communities, often influenced by traditional health beliefs. It is crucial for clinicians to respect these perspectives while offering evidence‑based recommendations. Engaging patients in shared decision‑making can bridge the gap between modern medicine and cultural practices, fostering adherence and better health outcomes.
Tina Johnson May 17, 2023 at 01:25
Honestly, the literature is saturated with hype. Budesonide helps, but you’ll still need to undergo multiple endoscopies and adhere to strict dietary restrictions. It’s not a magic bullet, and patients often overlook the importance of follow‑up. Adjustments in dosage are common, so be prepared for ongoing tweaks.
Sharon Cohen May 17, 2023 at 08:22
Ah, the drama of another “miracle” steroid-watch the hype train arrive! Budesonide does the job, sure, but it’s no Hollywood ending. You’ll still wrestle with the daily grind of dosing, storage, and that inevitable taste that clings to your throat. Slip-ups happen, and the inflammation loves to make a comeback like an old rival. So, brace yourself for the endless cycle of appointments, biopsies, and the occasional side‑effect cameo. Yet, in the midst of this theatrical saga, there’s a sliver of hope: many patients finally swallow without fear. That, my friends, is the modest applause we can expect.
Rebecca Mikell May 17, 2023 at 13:55
I appreciate the candid perspective. While the process can feel like a marathon, the incremental improvements-like being able to enjoy a simple piece of toast-are truly rewarding. Collaboration between the patient and healthcare team makes all the difference.
Ellie Hartman May 17, 2023 at 18:05
Exactly! It’s all about steady steps and a supportive environment. Celebrate those small victories, and don’t hesitate to lean on your support network when the journey feels tough.