Understanding Amenorrhea and Its Types
Amenorrhea is a medical term that refers to the absence of menstruation – a woman's monthly period. It's important to note that amenorrhea can be categorized into two types: primary and secondary amenorrhea. Primary amenorrhea occurs when a female has not started menstruating by the age of 16, while secondary amenorrhea is defined as the absence of menstruation for at least three consecutive cycles after a woman has already started having her period.
Many factors can contribute to amenorrhea, such as hormonal imbalances, stress, excessive exercise, or certain medical conditions. One such medical condition is Polycystic Ovary Syndrome (PCOS), which often leads to hormonal imbalances and can cause amenorrhea. In this article, we will explore the connection between amenorrhea and PCOS, discuss the symptoms of both conditions, and delve into possible treatments and management options.
Exploring the Symptoms of Polycystic Ovary Syndrome (PCOS)
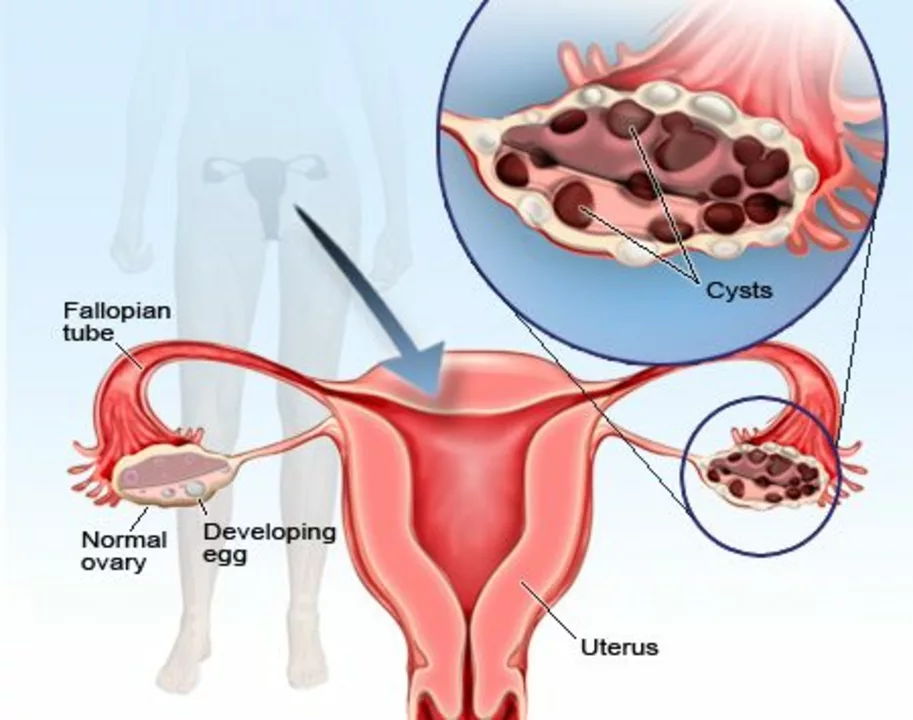
PCOS is a common hormonal disorder that affects women of reproductive age. It is characterized by the presence of multiple small cysts on the ovaries, which can lead to irregular menstrual cycles, excessive hair growth, acne, and obesity. The exact cause of PCOS is unknown, but it is believed to be linked to insulin resistance and abnormal hormone levels.
Common symptoms of PCOS include:
- Irregular periods or complete absence of periods
- Excessive hair growth on the face, chest, back, or buttocks
- Acne or oily skin
- Weight gain or difficulty losing weight
- Thinning hair or male-pattern baldness
- Darkening of the skin, particularly around the neck, groin, and under the breasts
How PCOS Contributes to Amenorrhea
One of the main reasons behind the connection between amenorrhea and PCOS is the hormonal imbalances associated with the latter. Women with PCOS often have higher levels of androgens – male hormones that can affect the menstrual cycle and cause the ovaries to enlarge and form small cysts. This can lead to irregular periods or amenorrhea.
Another contributing factor is insulin resistance, commonly seen in women with PCOS. Insulin resistance can further disrupt hormonal balance, affecting the menstrual cycle and leading to amenorrhea. Lastly, obesity, which is often linked to PCOS, can also contribute to the development of amenorrhea due to its impact on hormone levels and menstrual function.
Diagnosing PCOS and Amenorrhea
If you suspect you have PCOS or amenorrhea, it's essential to consult a healthcare professional to get a proper diagnosis. Your doctor will likely perform a physical examination, discuss your medical history, and may order blood tests to check hormone levels. In some cases, an ultrasound may be performed to examine the ovaries and check for cysts.
It's important to note that diagnosing PCOS can be challenging, as its symptoms can be similar to other conditions, such as thyroid disorders or adrenal gland issues. Your doctor will take this into consideration and may perform additional tests to rule out other potential causes of your symptoms.
Treatment and Management Options for Amenorrhea and PCOS
While there is no cure for PCOS, there are various treatment options to help manage its symptoms and reduce the risk of complications, such as infertility, type 2 diabetes, and heart disease. Treatment plans for PCOS and amenorrhea often focus on addressing hormonal imbalances, improving insulin resistance, and promoting a healthy lifestyle.
Some common treatment options include:
- Birth control pills or hormonal therapy to regulate the menstrual cycle and reduce androgen levels
- Anti-androgen medications to help reduce excessive hair growth and acne
- Metformin, a medication that improves insulin resistance and may help with weight loss
- Lifestyle changes, such as adopting a healthy diet, regular exercise, and stress reduction techniques
- Fertility treatments, if pregnancy is desired
It's crucial to work closely with your healthcare team to devise a treatment plan tailored to your specific needs and symptoms. With the appropriate care and management, women with PCOS and amenorrhea can lead healthy, fulfilling lives.
Comments
Jai Patel May 5, 2023 at 23:09
Let’s cut to the chase-hormonal chaos is the real villain behind missed periods, and PCOS loves to stir that pot. When insulin resistance slips in, it drags estrogen and androgen levels into a wild tango that can shut down the uterine lining. The good news? Lifestyle tweaks like balanced carbs and steady cardio can tame that beast, nudging cycles back on track. Pair that with a smart doc’s prescription-maybe metformin or birth‑control-and you’ve got a solid game plan. Keep the stress dial low, and watch your body find its rhythm again.
Zara @WSLab May 8, 2023 at 06:42
💪 You’ve got this! Managing PCOS is all about steady steps, not lightning‑fast fixes. A mix of gentle exercise and a wholesome diet can smooth out insulin spikes and bring those cycles back. 🌸 Remember, every tiny win adds up to big confidence.
Randy Pierson May 10, 2023 at 14:16
Here’s the lowdown: PCOS often throws off the delicate feedback loop between the hypothalamus and ovaries, which can silence the menstrual orchestra. Think of it as a mis‑tuned instrument; the body just can’t keep the beat. Restoring balance with a combo of hormonal therapy and lifestyle changes rewires the system. Don’t forget to get those blood panels done; they’re the map to your hormone terrain. Consistency is key-your body rewards steady, healthy habits.
Bruce T May 12, 2023 at 21:49
Honestly, it’s a bit shocking how many people overlook the moral duty of taking care of their own health. Ignoring PCOS symptoms is like turning a blind eye to a ticking time‑bomb for diabetes and heart disease. You owe it to yourself to get proper testing and treatment. No excuses, just action.
Darla Sudheer May 15, 2023 at 05:22
PCOS can feel like a fog but a simple blood test clears it up. Regular check‑ups help spot hormone swings early. A balanced diet and some movement go a long way-trust me.
Elizabeth González May 17, 2023 at 12:56
It is imperative to recognize that amenorrhea, when contextualized within the framework of polycystic ovary syndrome, represents not merely a symptom but a profound indicator of systemic endocrine dysregulation. The oscillation of androgenic activity, which typifies PCOS, exerts a suppressive effect upon the hypothalamic‑pituitary‑ovarian axis, thereby attenuating the luteinizing hormone surge requisite for ovulation. Consequently, the endometrial lining fails to undergo the proliferative‑secretory transformation that culminates in menses. Moreover, insulin resistance, a prevalent comorbidity in PCOS, amplifies hyperinsulinemia, fostering ovarian theca cell hyperactivity and further exacerbating hyperandrogenism. This multifaceted hormonal milieu engenders a cascade wherein follicular arrest, anovulation, and ultimately amenorrhea become almost inevitable. Clinicians must therefore adopt a holistic investigative approach, integrating serum androgen concentrations, fasting glucose, and oral glucose tolerance testing to elucidate the underlying metabolic perturbations. Imaging, typically via transvaginal ultrasonography, offers corroborative evidence of polycystic morphology, yet it remains secondary to the biochemical profile. Therapeutic interventions, accordingly, should prioritize insulin sensitization through agents such as metformin, alongside hormonal regulation achieved via combined oral contraceptives. Lifestyle modification, encompassing dietary glycemic control and aerobic exercise, constitutes an essential adjunct, as it mitigates both weight gain and insulin resistance. Patient education is paramount; individuals should be apprised of the long‑term sequelae, including type 2 diabetes mellitus, dyslipidemia, and cardiovascular risk. In addition, psychological support is often warranted, given the distress associated with infertility and chronic amenorrhea. Regular follow‑up enables dynamic adjustment of treatment regimens, ensuring optimal endocrine equilibrium. Ultimately, the convergence of precise diagnosis, individualized therapy, and sustained patient engagement fosters the restoration of menstrual cyclicity and the amelioration of PCOS‑related morbidities. Therefore, a comprehensive, interdisciplinary strategy remains the cornerstone of effective management.
chioma uche May 19, 2023 at 20:29
Our nation’s women deserve better than vague advice; we need public health policies that fund PCOS screening in schools and workplaces. Ignoring the prevalence of amenorrhea is an injustice to our future generations. Let’s demand action from the Ministry of Health now.
Satyabhan Singh May 22, 2023 at 04:02
In contemplating the interplay between amenorrhea and PCOS, one must adopt a perspective that transcends mere clinical observation, delving into the philosophical dimensions of bodily autonomy. The dysregulation of endocrine pathways reflects a broader narrative of balance and discord within the human organism. By fostering an environment that encourages both scientific rigor and compassionate care, we may yet restore the harmonious rhythm of the menstrual cycle. It is through such a synthesis of intellect and empathy that we shall advance our understanding.
Keith Laser May 24, 2023 at 11:36
Look, it’s not rocket science-PCOS messes with hormones, and then your period decides to take a vacation. The silver lining? You can actually beat it with a mix of meds and lifestyle tweaks, no miracle powders needed. And hey, if someone tells you it’s "just a phase," you can politely roll your eyes and move on. Keep your head up, stay consistent, and let the doctors do their thing.
Winnie Chan May 26, 2023 at 19:09
Seriously, the whole “just wait for it to fix itself” vibe is the worst. You’ve got a condition that needs a plan, not a wish. A little humor helps-think of your cycle like a mischievous cat that needs coaxing with the right treats. Stay proactive and give it the TLC it deserves.
Kyle Rensmeyer May 29, 2023 at 02:42
They don’t tell you that the pharma giants are pushing pills to keep us buying forever :) but truth is PCOS is a trap set up by deep‑state health agendas 😒 get tested and don’t trust everything they say
Rod Maine May 31, 2023 at 10:16
Yo PCOS is a total buzzkill.
Othilie Kaestner June 2, 2023 at 17:49
Honestly, all this “lifestyle change” hype is just a distraction from the fact that our bodies are being weaponized by Western diet propaganda. PCOS isn’t a personal failing; it’s a symptom of a broken system. Stop blaming women for their hormones and start fixing the food industry.
Sebastian Samuel June 5, 2023 at 01:22
Hey, I’ve been feeling super drained lately and the doctor says it’s PCOS 😩. It’s like my energy just leaks out, and I can’t even enjoy a good meme night 🎭. If anyone has tried mixing yoga with a low‑carb plan and actually felt better, spill the tea 😊.
Mitchell Awisus June 7, 2023 at 08:56
First, ensure you get a comprehensive hormonal panel; this will pinpoint the specific imbalances at play. Second, discuss with your endocrinologist the possibility of metformin to improve insulin sensitivity. Third, consider a low‑glycemic diet-think whole grains, legumes, and plenty of vegetables. Fourth, incorporate regular, moderate exercise, such as brisk walking or cycling, to aid weight management. Finally, maintain open communication with your healthcare team to adjust treatment as needed; consistent follow‑up is essential for long‑term success.