What Is Steroid Myopathy?
Steroid myopathy is a muscle-wasting condition caused by long-term use of corticosteroids like prednisone, dexamethasone, or cortisone. It’s not an infection or autoimmune disease-it’s a direct toxic effect on muscle tissue. First noticed in the 1930s in patients with Cushing’s syndrome, it’s now one of the most common drug-related muscle problems worldwide. Unlike muscle pain from injury or inflammation, steroid myopathy causes painless weakness, often going unnoticed until daily tasks become impossible.
Who Gets It and When?
You don’t need to be on high doses for years to develop this. Taking more than 10 mg of prednisone daily for four weeks or longer raises your risk. In hospitals, patients on IV steroids like dexamethasone can show symptoms in just two to three weeks. People with asthma, COPD, rheumatoid arthritis, lupus, or those on long-term treatment for autoimmune disorders are most at risk. Dexamethasone is especially likely to cause muscle loss compared to other steroids, particularly in cancer treatments like acute lymphoblastic leukemia.
What’s scary is how often it’s missed. Up to 40% of cases are mistaken for disease progression or just being out of shape. Doctors might assume your weakness comes from your original condition-not the medicine helping it. A 2019 study found that 78% of patients with normal manual muscle tests actually had measurable strength loss when tested with machines. If you’ve been on steroids for months and feel like you’re losing grip on everyday life, it’s worth asking: Could this be steroid myopathy?
How Does It Feel? The Real Signs
The weakness doesn’t come with pain, swelling, or cramps. That’s why it sneaks up on you. You start noticing things you never had trouble with before:
- Needing your arms to push off the armrests to stand up from a chair
- Having to hold onto the handrail when climbing stairs
- Being unable to lift your arms to reach a high shelf or brush your hair
- Feeling like your legs are heavy, even after resting
This isn’t just feeling tired. It’s proximal muscle weakness-meaning the muscles closest to your body’s center (hips, thighs, shoulders) are affected first. The pelvic girdle (hips and thighs) weakens before the shoulders. That’s why getting up from a low chair feels impossible without using your hands. Patients on support forums describe it as "feeling like your legs are made of concrete."
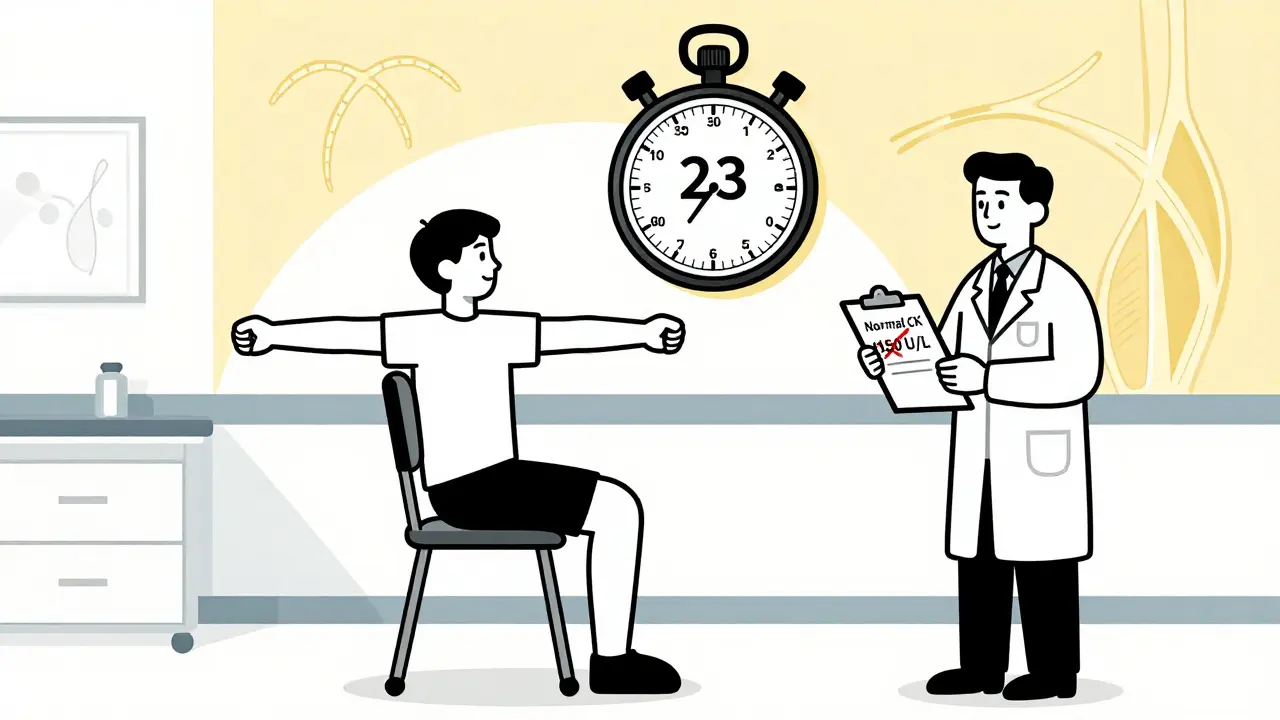
How Is It Diagnosed?
There’s no single blood test for steroid myopathy. In fact, the most telling thing is what’s not there. Your creatine kinase (CK) levels-the enzyme that spikes when muscles break down-are usually normal (30-170 U/L). In inflammatory muscle diseases like polymyositis, CK levels soar above 500 U/L. That’s a key difference.
Electromyography (EMG) tests also look normal, unlike in inflammatory conditions where you see "early recruitment" patterns. A muscle biopsy is the gold standard: it shows shrinkage of type 2b fast-twitch muscle fibers-the ones responsible for power and quick movements-with no signs of inflammation. That’s why steroid myopathy is called a "noninflammatory myopathy."
Doctors use functional tests to catch it early:
- Timed chair rise test: How long does it take to stand up from a chair five times without using your arms? Normal is under 10 seconds. People with steroid myopathy often take 20 seconds or more.
- Gower’s maneuver: Can you get up from the floor without using your hands? If you have to crawl up using your arms, that’s a red flag.
- Shoulder abduction test: Can you lift your arms sideways to shoulder height? Weakness here is a classic sign.
These tests are simple, quick, and more accurate than standard strength checks. Yet, only 27-32% of rheumatology and pulmonology clinics use them routinely. If you’re on long-term steroids, ask for one.
Why Resistance Training Works-And Why High Intensity Doesn’t
Resting won’t fix this. Neither will stretching or light walking. What helps is targeted resistance training. But not just any training. Steroid myopathy breaks down muscle faster than your body can rebuild it. You need to stimulate muscle growth without tearing it apart.
A 2020 clinical trial showed patients who did supervised resistance training three times a week improved their chair rise time by 23.7% in just 12 weeks. The control group, who didn’t train, improved by only 8.2%. No one got hurt. No one had muscle damage. That’s because the training was carefully dosed: 40-60% of your one-rep maximum, starting low and increasing slowly.
Here’s what works:
- Start with 30% of your max strength-maybe bodyweight squats, seated leg presses, or wall push-ups
- Do 2-3 sets of 10-15 reps, 2-3 times per week
- Progress by adding 5-10% resistance every two weeks, only if you feel no soreness or fatigue the next day
- Focus on hip extension (bridges), knee extension (leg extensions), and shoulder abduction (light dumbbell raises)
Avoid heavy lifting, high-intensity interval training, or anything that leaves you exhausted. Overdoing it can trigger more muscle breakdown. The goal isn’t to get stronger fast-it’s to rebuild what the steroids took away, slowly and safely.
What About Stopping the Steroids?
Many patients think stopping the steroid will fix the weakness. But that’s not always possible-or safe. If you have lupus, asthma, or rheumatoid arthritis, your doctor prescribed steroids because they’re life-saving. Stopping them abruptly can trigger a flare-up worse than the muscle weakness.
The good news? Muscle recovery starts even while you’re still on steroids. Studies show strength improves with exercise regardless of steroid use. In fact, continuing low-dose steroids while doing resistance training is safer than stopping them cold. Your physical therapist will work with your doctor to balance your treatment.
What’s New in Treatment?
Researchers are working on drugs that keep the anti-inflammatory benefits of steroids but cut the muscle damage. One promising compound, Vamorolone, is in Phase II trials. In early results, patients taking it had 40% less muscle weakness than those on regular prednisone at the same dose. It’s not available yet, but it’s a sign that the medical community is finally taking this problem seriously.
The 2023 International Myopathy Guidelines Consortium is also developing the first official physical therapy protocols for steroid myopathy. That means standardized care-no more guessing what works.

Why This Matters More Than You Think
Prednisone is the 34th most prescribed drug in the U.S.-17.8 million prescriptions in 2022. Millions of people are on it. And for every one who gets diagnosed with steroid myopathy, three more go undetected. The cost isn’t just physical. People with this condition fall more often, need more rehab, and spend $1,200-$2,400 extra per year on healthcare.
But here’s the real truth: You don’t have to accept this weakness. It’s not "just part of getting older" or "what happens when you’re sick." It’s a known, treatable side effect. The tools to fix it exist. The science is clear. What’s missing is awareness.
What You Can Do Today
- If you’ve been on steroids for more than a month and feel weaker, ask your doctor for a timed chair rise test.
- Request a referral to a physical therapist who understands drug-induced myopathy.
- Start with gentle resistance exercises-bodyweight squats, seated leg lifts, wall push-ups. Do them 2-3 times a week.
- Track your progress: Write down how long it takes to stand from a chair without using your arms. Do it every two weeks.
- Don’t stop your steroids without talking to your doctor.
Recovery isn’t about going back to how you were before. It’s about rebuilding strength, one small step at a time-while still managing the condition that made you need steroids in the first place.
Can steroid myopathy be reversed?
Yes, in most cases. Muscle strength improves with consistent, moderate resistance training-even while still taking steroids. Recovery takes weeks to months, but studies show up to 25% improvement in functional strength within 12 weeks. Complete reversal is possible if the steroid dose is reduced and exercise is maintained.
Does steroid myopathy cause muscle pain?
No. Unlike inflammatory muscle diseases, steroid myopathy is painless. You may feel fatigue or heaviness, but not soreness, cramps, or tenderness. Pain usually means something else is going on-like an infection or another type of myopathy-and should be checked by a doctor.
Is steroid myopathy the same as muscle wasting from aging?
No. Age-related muscle loss (sarcopenia) affects all muscle fibers slowly over years. Steroid myopathy targets fast-twitch type 2b fibers specifically and develops much faster-often within weeks. It also affects younger people on long-term steroids, not just older adults.
Can physical therapy help if I’m on high-dose steroids?
Yes. In fact, physical therapy is especially important for patients on high doses, including those in intensive care. Studies show that even patients on IV steroids benefit from gentle, supervised resistance training. The key is starting low-30% of your max strength-and progressing slowly. Avoid overexertion.
How long does it take to see improvement with physical therapy?
Most patients notice small improvements in daily function-like standing from a chair without help-within 4 to 6 weeks. Measurable gains in strength, confirmed by tests like the timed chair rise, typically appear after 8 to 12 weeks of consistent training. Patience and consistency matter more than intensity.
Are there any supplements that help with steroid myopathy?
No supplement has been proven to reverse steroid myopathy. While protein intake and vitamin D are important for general muscle health, they won’t fix the problem alone. The only proven intervention is targeted resistance training. Avoid unregulated "muscle-building" supplements-they can interfere with your medications or cause liver damage.
Next Steps: What to Do Now
If you’re on corticosteroids and feeling weaker, don’t wait. Talk to your doctor about a functional strength test. Ask for a referral to a physical therapist experienced in neuromuscular conditions. Start with simple, safe movements at home-like seated leg lifts or wall push-ups. Track your progress. You’re not just fighting a side effect-you’re reclaiming your ability to move, stand, and live without help.
Comments
Cameron Hoover December 21, 2025 at 02:45
I was on prednisone for 6 months after my lung flare-up. Thought I was just getting old or lazy. Then I couldn't get up from my couch without using my arms. Started doing wall push-ups and seated leg lifts like the article said. 8 weeks later, I'm back to climbing stairs without holding the rail. It's not magic-it's just science you didn't know about. Don't give up.
Sandy Crux December 21, 2025 at 08:26
The article is... *admirably* thorough, yet profoundly naive. It presumes that resistance training is universally accessible, ignoring socioeconomic barriers, disability status, and the fact that many patients are too frail to even attempt it. Also, why is there no mention of the pharmaceutical-industrial complex's disincentive to promote non-pharmaceutical interventions? The real issue isn't the myopathy-it's the system that lets it go undiagnosed for decades.
Hannah Taylor December 22, 2025 at 14:55
lol they never tell you the real reason steroids wreck your muscles. it's not the drug-it's the glyphosate in your food + 5G radiation messing with your mitochondria. i read this on a forum where a guy said his dog got weaker after the vet gave it prednisone... then he found out the vet's office was near a cell tower. coincidence? i think not. also, vitamin d3 k2 is the real fix. no one wants you to know that.
Jason Silva December 24, 2025 at 13:09
I was skeptical but tried the chair rise test after reading this. Took me 22 seconds. I cried. Then I started doing bodyweight squats every morning. 12 weeks later? 8 seconds. No joke. This saved my life. 🙏💪
mukesh matav December 24, 2025 at 16:19
Interesting. I am on steroids for my arthritis. I did notice my legs feel heavy. But I thought it was just because I sit too much. Maybe I will try the simple exercises. Thank you for sharing.
Peggy Adams December 25, 2025 at 20:10
Ugh. Another one of those 'just do some squats' articles. Like I don't have 3 kids, a full-time job, and a doctor who won't listen. I don't have time to 'track my progress.' And no, I'm not going to start lifting weights when I can barely walk to the fridge.
Sarah Williams December 26, 2025 at 22:38
This is exactly what I needed. I've been telling my rheumatologist for months that I'm losing strength-but they kept saying 'it's your lupus.' I asked for the chair test last week. Took 24 seconds. They were shocked. PT referral is scheduled. You're not alone. Keep going.
Theo Newbold December 28, 2025 at 05:27
The data presented is statistically sound but methodologically limited. The sample sizes in the cited trials are small, selection bias is unaddressed, and there's no control for concurrent medications or nutritional status. The conclusion that resistance training is 'the only proven intervention' is premature. Until longitudinal RCTs with biomarker validation are published, this remains anecdotal correlation masquerading as clinical guidance.
Jay lawch December 29, 2025 at 01:44
You think this is about muscles? No. This is about the globalist agenda to weaken the population. Steroids are just the vehicle. The real goal is to make you dependent on machines, therapists, and government-approved exercises so they can track your movement patterns. Why do you think they never mention the real solution? The ancient Indian practice of surya namaskar-12 sun salutations daily-was used for millennia to rebuild strength without drugs. But no, we must follow Western protocols. They don't want you to know the truth. They fear the power of yoga. I've been doing it for 3 months. My strength is returning. The system hates this.
Erika Putri Aldana December 30, 2025 at 09:10
I don't care what the article says. I'm not doing squats. I'm not doing anything. I just want my meds and my couch. Why do people act like you have to 'fix' everything? Sometimes you just gotta rest. And if you're weak, you're weak. Deal with it.
Adrian Thompson December 31, 2025 at 02:28
Prednisone is a weaponized drug. The FDA knows this. The pharma reps know this. Your doctor knows this. But they still prescribe it like it's aspirin. Why? Because they get kickbacks. And now they want you to do 'resistance training' so they don't have to admit the drug is toxic? No thanks. I'm switching to CBD oil and fasting. That's the real solution. The system is rigged.
Teya Derksen Friesen January 1, 2026 at 05:08
The meticulous articulation of functional assessment protocols is both commendable and overdue. One must, however, underscore the imperative of individualized progression parameters, particularly in geriatric or multimorbid populations. The prescribed 30% of one-rep maximum is an excellent starting point, yet concurrent monitoring of inflammatory markers and functional mobility scales remains essential to mitigate iatrogenic risk. A most prudent and evidence-based contribution to the literature.
Southern NH Pagan Pride January 1, 2026 at 17:46
i found out my dr is on the payroll of the big pharma corpz. they told me to do 'resistance trainin' but they dont want me to stop the steroids because they make billions. i started doing yoga in my backyard at sunrise. i also stopped eating gluten and dairy. my strength came back. the system is scared of people like me. they dont want you to know you can heal without their pills.