When you hear about semaglutide, you’re probably hearing about people losing 20, 30, even 50 pounds - and doing it without surgery. But here’s the truth: semaglutide isn’t a magic pill. It’s a powerful tool, and like any tool, it only works if you understand how to use it - and what the real costs are.
What Semaglutide Actually Does in Your Body
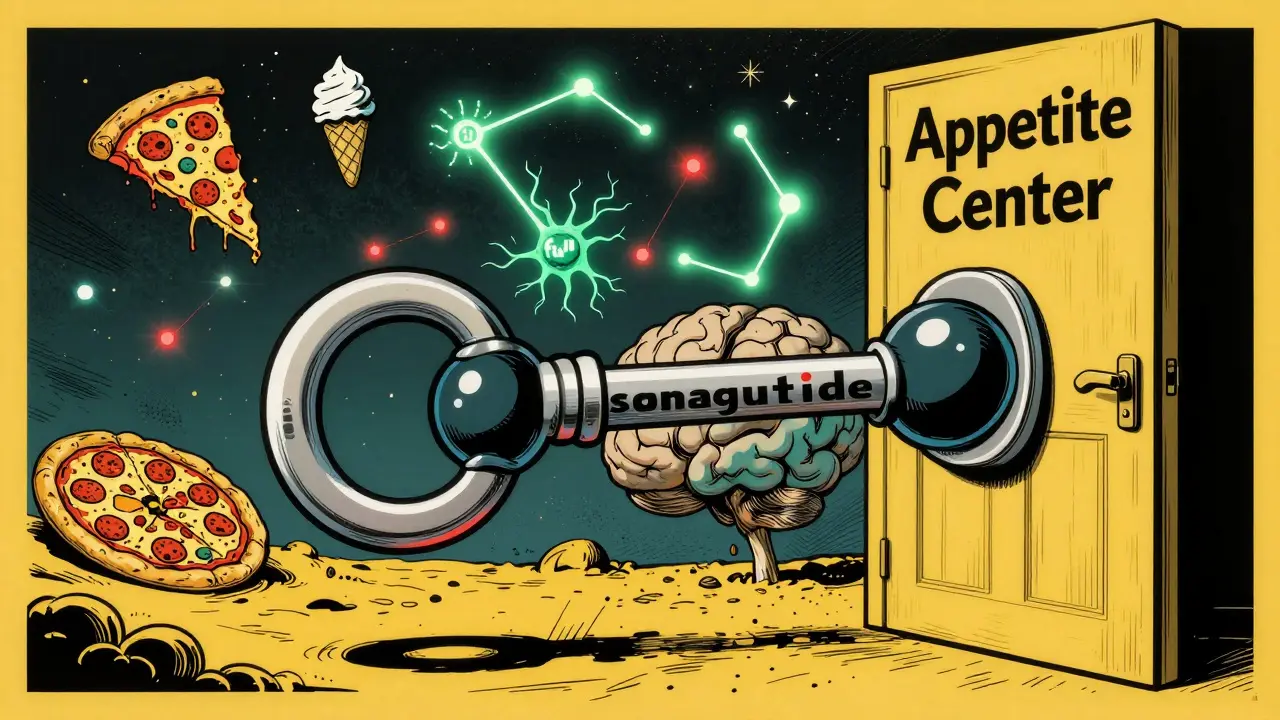
Semaglutide isn’t just another appetite suppressant. It mimics a hormone your body already makes called GLP-1, which tells your brain when you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin only when needed. That’s why it works so well for both diabetes and weight loss.In the STEP 1 clinical trial, people using Wegovy lost an average of 14.9% of their body weight over 68 weeks. That’s not a small number - it’s the kind of loss most people only see after gastric bypass surgery. Compare that to placebo, where people lost just 2.4%. The difference? Nearly 13 percentage points. And 79% of those on semaglutide lost at least 10% of their weight. Only 12% of the placebo group did.
It doesn’t just make you eat less. It changes how your brain sees food. People on semaglutide report that high-calorie foods - pizza, ice cream, fried chicken - just don’t feel as appealing. You don’t feel deprived. You just… don’t crave it as much. That’s the real shift.
Ozempic vs Wegovy: Same Drug, Different Doses
Ozempic and Wegovy are both semaglutide. The active ingredient is identical. The only real difference? The dose and what the FDA approved them for.Ozempic was first approved in 2017 for type 2 diabetes, at doses up to 1.0 mg weekly. Wegovy came later, in 2021, with a higher dose - 2.4 mg weekly - specifically for weight loss. So if you’re on Ozempic for diabetes and your doctor ups your dose to 1.7 mg or 2.0 mg, you might lose weight as a side effect. But Wegovy is the only version legally approved for weight loss alone.
Here’s the kicker: the higher dose in Wegovy delivers more consistent results. In head-to-head studies, semaglutide at 2.4 mg (Wegovy) led to about 15% weight loss. Liraglutide (Saxenda), another GLP-1 drug, maxed out at around 8%. That’s not even close.
Why It Works So Well - And Why It’s Not Perfect
Semaglutide doesn’t just turn off hunger. It talks to your brain’s appetite center, the hypothalamus. It activates neurons that say, “You’re full,” and shuts down ones that scream, “Eat more.” It also works with leptin, the hormone your fat cells release, to amplify the signal. Think of it as a team effort: your body’s natural signals, boosted by the drug.It also slows digestion. Food sits in your stomach longer. Blood sugar spikes less after meals. That’s why people feel more stable energy and fewer cravings. But this same mechanism causes the side effects everyone talks about: nausea, vomiting, diarrhea. About 77% of users get nausea. 64% get diarrhea. 56% vomit. Most of these fade after a few weeks - if you stick to the slow dose escalation.
That’s why the dosing schedule matters. Wegovy starts at 0.25 mg once a week. You stay there for four weeks. Then you go to 0.5 mg. Then 1.0 mg. Then 1.7 mg. Finally, 2.4 mg. It takes 16 to 20 weeks to reach the full dose. Rushing it? You’ll likely quit because you feel sick. Patience is part of the treatment.
What Happens When You Stop?
This is the part no one tells you until it’s too late.Studies show that when people stop semaglutide, they regain about two-thirds of the weight they lost within a year. In the STEP 4 trial, those who switched from semaglutide to placebo regained 6.9% of their body weight. Those who kept taking it held onto 10.6% loss. That’s not a coincidence. The drug doesn’t fix the underlying biology of obesity - it manages it.
Think of it like high blood pressure medication. You don’t stop taking it because your pressure drops. You keep taking it because the condition doesn’t go away. Obesity is a chronic disease. Semaglutide treats it, but it doesn’t cure it.
And here’s the painful reality: most people stop because they can’t afford it or can’t get it. Insurance often denies coverage unless you have diabetes or cardiovascular disease. In the U.S., Wegovy costs about $1,350 a month without insurance. That’s $16,200 a year. Many patients report being on waiting lists for months, or getting partial doses because pharmacies are out of stock.
Who Benefits Most - And Who Should Avoid It
Semaglutide works best for adults with a BMI of 30 or higher, or 27 or higher with at least one weight-related condition like high blood pressure, sleep apnea, or prediabetes. It’s especially effective in people without diabetes - 86% of non-diabetic STEP trial participants lost at least 10% of their weight.But it’s not for everyone. If you or a family member has medullary thyroid cancer or Multiple Endocrine Neoplasia Type 2, you can’t take it. Rodent studies showed thyroid tumors at high doses. Human risk is still unclear, but the FDA requires a REMS program to warn doctors and patients.
It’s also not a substitute for lifestyle changes. The STEP trials included weekly counseling on diet and exercise. People who combined semaglutide with better food choices and movement lost more - and kept it off longer. The drug helps you eat less. But if you still eat processed junk, you won’t get the full benefit.

What’s Next? New Drugs, New Hope
Semaglutide isn’t the end of the story. Tirzepatide (Zepbound), a dual GLP-1 and GIP agonist, showed even better results - up to 20.9% weight loss in trials. That’s more than Wegovy. Oral semaglutide (Rybelsus) is approved for diabetes, but early trials for weight loss show about 10.9% loss - less than the injectable, but still meaningful.Novo Nordisk is now testing semaglutide in teens aged 12 to 17. If approved, this could change how we treat childhood obesity. And there’s talk of combining semaglutide with other drugs to boost results and reduce side effects.
But here’s the hard truth: even if these drugs work better, they won’t solve the obesity crisis unless we fix access. Right now, only a fraction of people who could benefit can get them. And even if they do, most can’t afford to stay on them forever.
Real People, Real Results
On Reddit’s r/Ozempic community, with over 125,000 members, stories range from life-changing to heartbreaking. One user wrote: “I lost 40 pounds and kept it off for 18 months with Wegovy and walking 30 minutes a day.” Another said: “The nausea was so bad I had to quit at 1.7 mg.”On Drugs.com, Wegovy has a 7.9 out of 10 rating. Sixty-eight percent of reviewers say it helped. But on Trustpilot, the rating is only 2.1 out of 5 - mostly because people couldn’t get their prescription filled or insurance denied coverage.
The pattern is clear: those who can access the drug and stick with it, often with support, see huge gains. Those who can’t - whether because of cost, side effects, or supply issues - are left behind.
What You Should Do If You’re Considering Semaglutide
1. Talk to a doctor who specializes in obesity medicine. Not every provider knows how to use these drugs properly.2. Ask about your insurance coverage. Many insurers require proof of failed diet attempts, a BMI over 30, and a weight-related condition.
3. Be ready for side effects. Start low. Go slow. Don’t skip the dose escalation.
4. Pair it with lifestyle changes. No drug replaces movement, sleep, or balanced eating.
5. Plan for the long term. If you stop, expect to regain weight. Decide now: are you prepared to stay on this indefinitely?
6. Check for patient assistance programs. Novo Nordisk offers support for uninsured or underinsured patients.
Semaglutide has changed the game. For the first time, we have a drug that can help people lose weight - and keep it off - without surgery. But it’s not a quick fix. It’s a long-term commitment. And until we fix the cost and access problems, it will remain a miracle drug for the few, not a solution for the many.

Comments
Aliza Efraimov December 30, 2025 at 14:44
I lost 37 pounds on Wegovy and kept it off for two years. Not because I’m disciplined-because the cravings just vanished. Pizza used to be my emotional anchor. Now? I look at it and think, ‘That’s a lot of calories for zero joy.’ It didn’t make me hungry-it made me indifferent. That’s the real magic.
But yeah, the nausea? Brutal. I cried in the bathroom for three weeks. Slow escalation saved me. Don’t rush it. Your stomach will thank you.
And no, it’s not a cure. It’s a tool. Like a wheelchair for someone with mobility issues. Doesn’t mean you stop moving. It means you can move at all.
Insurance denied me twice. I paid out of pocket for six months. Worth every penny. I can now play with my niece without gasping for air.
If you’re considering this, find an obesity specialist. Not your general doc. They don’t get it.
And if you’re on it and feeling guilty? Stop. You’re not lazy. You’re managing a chronic disease. Like diabetes. Like hypertension. You wouldn’t shame someone for taking insulin.
I’m not a doctor. Just someone who got their life back.
Nisha Marwaha January 1, 2026 at 09:29
From a clinical pharmacology standpoint, semaglutide’s mechanism of action as a GLP-1 receptor agonist is profoundly efficacious due to its prolonged half-life and high receptor affinity. The STEP trials demonstrated statistically significant reductions in adiposity metrics, with a mean weight loss of 14.9% versus placebo (p < 0.001). The pharmacokinetic profile supports once-weekly dosing, with peak plasma concentrations achieved at approximately 3 days post-injection.
Notably, the 2.4 mg dose of Wegovy achieves a greater receptor occupancy threshold than Ozempic’s 1.0 mg, resulting in enhanced satiety signaling via hypothalamic POMC neuron activation. The concomitant slowing of gastric emptying is mediated by vagal afferent modulation, which explains the GI side effect profile.
However, the real-world adherence challenges are non-trivial. Bioavailability variability due to injection technique, patient-reported nausea, and economic barriers-particularly in low-income cohorts-significantly attenuate population-level efficacy. The drug is not a panacea; it is a pharmacological adjunct to behavioral intervention.
Future directions include combination therapies with GIP agonists (e.g., tirzepatide) and oral formulations to improve accessibility. The metabolic reset hypothesis remains compelling, but long-term data beyond 3 years are still lacking.
For clinicians: titrate slowly. For patients: pair with cognitive behavioral strategies. For policymakers: subsidize access. This isn’t vanity-it’s public health.
Paige Shipe January 1, 2026 at 11:30
People act like this is some miracle cure but let’s be real-this is just another way for Big Pharma to make billions while regular people get stuck on waiting lists. I’m not jealous, I’m just tired of seeing people post about their ‘weight loss journey’ like it’s some kind of spiritual awakening. You didn’t ‘transform,’ you took a drug.
And don’t get me started on the people who say they ‘don’t crave junk food anymore.’ Yeah, right. You just don’t have the energy to go to the grocery store. That’s not freedom, that’s exhaustion.
Meanwhile, my cousin has diabetes and can’t even get Ozempic because her insurance says she’s ‘not sick enough.’
And the side effects? Nausea, vomiting, diarrhea? That’s not ‘adjusting.’ That’s being poisoned.
They’re selling a drug like it’s a lifestyle brand. It’s not. It’s a chemical crutch. And the people who can’t afford it? They’re just supposed to sit there and wait while you post your before-and-after on Instagram.
Grow up.
Tamar Dunlop January 1, 2026 at 11:44
As a Canadian living with obesity for over two decades, I find the global disparity in access to semaglutide both heartbreaking and deeply unjust. In our publicly funded system, coverage is restricted to those with type 2 diabetes or severe comorbidities, leaving many without options.
While I applaud the scientific advancement, I am equally appalled by the commodification of health. The $1,350 monthly price tag is not a reflection of manufacturing cost-it is a reflection of market power. In Canada, we have the infrastructure to provide equitable access; we simply lack the political will.
I have watched friends weep over pharmacy waitlists and insurance denials. This is not a lifestyle trend. It is a medical necessity for millions. To treat it as a luxury is to dehumanize chronic illness.
Let us not confuse efficacy with equity. The science is sound. The ethics are not.
Perhaps the next breakthrough should not be a stronger agonist, but a more compassionate policy.
I remain hopeful-but not naive.
David Chase January 3, 2026 at 06:22
OMG THIS IS THE MOST IMPORTANT THING YOU’LL EVER READ TODAY!!! 😱
Y’all are acting like semaglutide is some kind of alien tech from Mars. It’s a GLP-1 AGONIST. It’s not magic. It’s SCIENCE. And if you’re mad you can’t get it, maybe stop eating donuts and start lobbying your congressman!!
I lost 52 lbs on Wegovy. I’m not a monster. I’m not a privileged snowflake. I’m a veteran with PTSD and insulin resistance. This drug gave me my life back. My kids can now hug me without me wheezing. That’s not a ‘journey.’ That’s survival.
And yes, I had nausea. So did I cry? Yes. Did I quit? NO. I lowered the dose. I waited. I pushed through. That’s called discipline. Not everyone has it. That’s fine. But don’t act like it’s the drug’s fault.
Also, why are we still talking about Ozempic? It’s NOT approved for weight loss. Stop being lazy. Get the right prescription. Or don’t. But don’t lie to yourself.
And if you’re saying ‘it’s just for rich people’-then fix the system. Don’t hate the tool. FIX THE SYSTEM.
Also, I’m a nurse. I’ve seen 87 patients on this. 82 are still on it. 5 quit because they wanted to eat cake again. Not the drug’s fault. 😎
Emma Duquemin January 5, 2026 at 05:32
Okay, I’m not a scientist, but I’m a mom who lost 48 pounds and finally felt like I could breathe again-and I’ve got to say, this drug didn’t just change my body, it changed my soul.
I used to eat when I was sad. Now? I just… feel sad. And I don’t need a cookie to fix it. That’s wild.
I cried the first time I walked into a store and didn’t have to ask for a bigger chair. I cried the first time my daughter hugged me without holding her breath. I cried the first time I wore jeans that didn’t pinch.
Yes, I got nauseous. Yes, I had to go slow. Yes, I paid $1,200 a month for six months before I got insurance. But here’s the thing: I didn’t just lose weight. I got my dignity back.
And if you think this is just about looks? You’re missing the point. This isn’t vanity. It’s freedom. It’s not being afraid to climb stairs. It’s not being the ‘fat friend’ at family events. It’s being able to be present in your own life.
I’m not a hero. I’m just someone who finally got a chance.
And if you’re on the waiting list? I see you. I’m rooting for you. Keep going. One week at a time. You’re not behind. You’re becoming.
Duncan Careless January 7, 2026 at 04:34
While the pharmacological efficacy of semaglutide is well-documented, I remain cautious about its long-term societal implications. The narrative surrounding these drugs often neglects the structural determinants of obesity-food deserts, economic stress, lack of access to physical activity infrastructure.
Pharmaceutical intervention, while valuable, should not supplant systemic reform. A person living in a food swamp cannot be expected to ‘choose better’ even with a GLP-1 agonist.
Additionally, the normalization of weight loss as a moral imperative risks stigmatizing those who cannot or will not use such drugs. Health is not synonymous with thinness.
My advice: Use this tool if it helps. But do not conflate its use with virtue. And advocate for policies that make healthy living possible for everyone-not just those who can afford $16,000 a year.
Respect the science. Respect the struggle. Respect the system that needs fixing.
Russell Thomas January 7, 2026 at 08:42
Wow. So let me get this straight. You’re telling me that if I just take a drug, I won’t want pizza anymore? And I’m supposed to believe that’s not just chemical brainwashing? That’s not healing-that’s sedation.
You people act like you’ve unlocked some ancient secret, but you’re just trading one addiction for another. One pill for another. One craving for another. You didn’t change your relationship with food-you just muted the signal.
And don’t give me that ‘it’s like insulin’ crap. Insulin doesn’t make you stop wanting cake. It just lets you live. This? This makes you stop caring.
And why are you all so proud of being numb? That’s not a win. That’s a surrender.
Meanwhile, my grandma lost weight by walking every day and eating home-cooked meals. No drug. No drama. Just life.
Maybe the problem isn’t your biology. Maybe it’s your culture.
Just saying.
Joe Kwon January 8, 2026 at 07:09
As someone who’s been on both sides of this-first as a skeptic, now as a patient-I want to say: this isn’t about being ‘good’ or ‘bad.’ It’s about biology.
I had tried every diet. Every program. Every cleanse. Nothing worked long-term. My body kept fighting me. Semaglutide didn’t make me lose weight-it let my body finally rest.
The nausea? Real. The cost? Unfair. The access? Broken.
But the science? Solid.
I’m not saying everyone needs this. But if you’re struggling and it’s not ‘laziness,’ it’s not ‘weakness,’ it’s not ‘lack of willpower’-it’s a metabolic disorder. And this drug treats the disorder.
Let’s stop shaming and start supporting. Let’s stop pretending it’s a trend and start treating it like the medical breakthrough it is.
And if you can’t get it? You’re not failing. The system is.
Let’s fix that. Together.
Nicole K. January 10, 2026 at 05:10
People are acting like this is some kind of miracle when it’s just another way to be selfish. You’re not ‘transforming’-you’re just avoiding responsibility. Why can’t you just eat less and move more? Everyone else does.
And now you want the government to pay for your drug so you can keep eating cake? No. That’s not fair. You should be ashamed.
My neighbor lost weight by walking her dog every day. She didn’t need a shot. She didn’t need a miracle. She just did the work.
Stop looking for shortcuts. Start being an adult.
This isn’t medicine. It’s an excuse.
Teresa Rodriguez leon January 10, 2026 at 15:03
I got on Wegovy last year. Lost 31 pounds. Stopped because I couldn’t afford it. Regained 20. Now I’m back on the waiting list. I don’t even cry anymore. Just numb.
My doctor said ‘try again next year.’
Good luck.
Manan Pandya January 12, 2026 at 14:43
As a physician in India, I’ve seen patients on semaglutide for both diabetes and weight loss. The results are remarkable-but the challenges are immense. Many patients cannot afford even the generic alternatives. Pharmacy shortages are common. The cultural stigma around obesity remains deeply entrenched.
However, I’ve also seen patients who, after starting treatment, begin to engage in physical activity for the first time in decades. One patient, a 58-year-old schoolteacher, started walking to work. Then she joined a yoga group. Then she volunteered at a community kitchen.
The drug didn’t change her. It gave her the space to change herself.
Let’s not reduce this to a pill. Let’s see it as a doorway.
And to those who say ‘just eat less’-have you ever tried to eat less when your body is screaming for energy? When every calorie feels like survival?
Compassion, not judgment, is the first medicine.