When Shingles is a painful rash caused by reactivation of the varicella‑zoster virus that also caused chickenpox, most people focus on the skin pain. But the virus can travel along the nerves that supply the eye, leading to serious vision threats. This guide shows exactly how shingles can affect your eyes, what early signs to watch for, and the steps you can take right now to keep your sight safe.
Key Takeaways
- Shingles can involve the eye in up to 15% of cases, called herpes zoster ophthalmicus.
- Early antiviral treatment within 72hours dramatically lowers the risk of permanent vision loss.
- The shingles vaccine reduces eye involvement by roughly 70% in adults over 50.
- Watch for red eye, pain, blurry vision, or a rash on the forehead/eyelid - these are warning signs.
- Prompt referral to an ophthalmologist and proper eye‑drop therapy are essential for recovery.
Understanding Shingles and the Eye
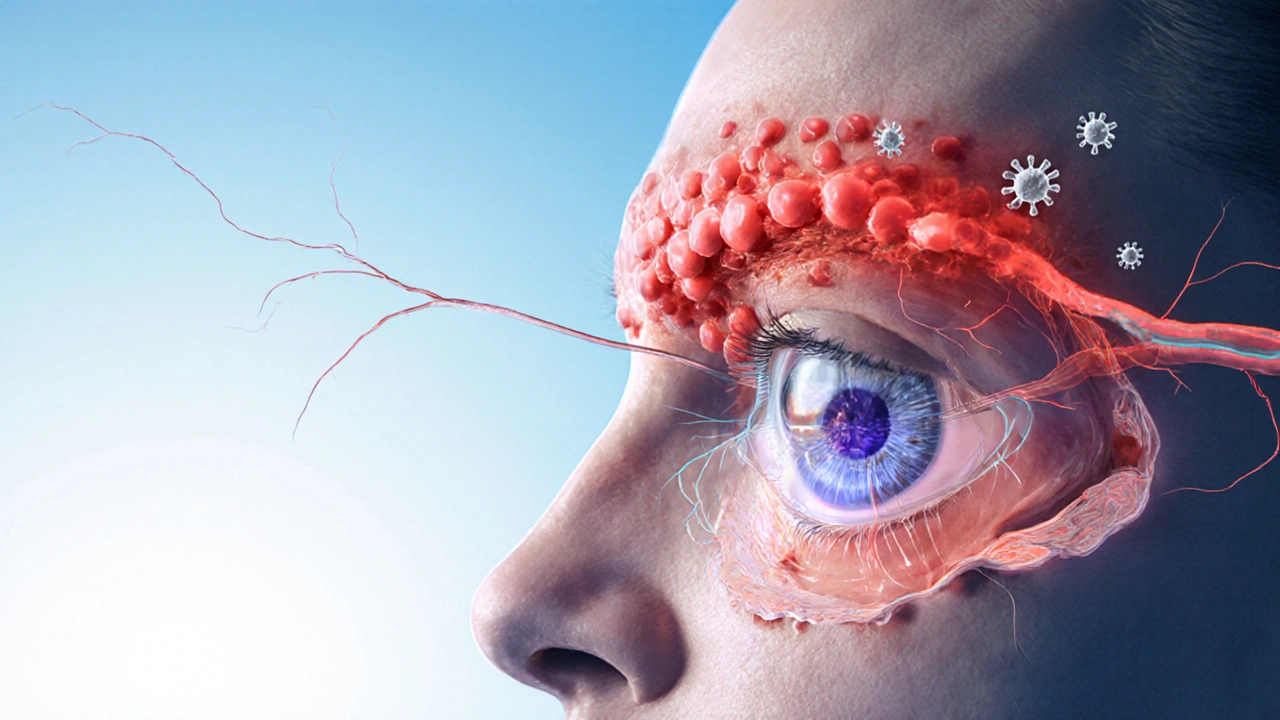
The culprit behind shingles is the Varicella‑zoster virus a herpesvirus that remains dormant in nerve ganglia after a childhood chickenpox infection. When immunity wanes, the virus can reactivate and travel down sensory nerves. If it travels down the ophthalmic branch of the trigeminal nerve, the condition is known as Herpes Zoster Ophthalmicus shingles affecting the eye and surrounding skin.
Why does this matter? The virus can directly infect delicate eye structures like the Cornea the clear front window of the eye that focuses light and the Retina the light‑sensing layer at the back of the eye. Inflammation (keratitis, uveitis, or retinitis) can scar tissue, leading to permanent vision loss if not treated promptly.
Who’s at Risk?
Anyone who’s had chickenpox can develop shingles, but certain groups see a higher eye‑involvement rate:
- Adults over 60 - immune defenses naturally decline.
- People with weakened immune systems (organ‑transplant recipients, HIV, chemotherapy patients).
- Individuals with a history of eye disease (glaucoma, prior infections).
- Those who haven’t received the shingles vaccine.
Even healthy 40‑year‑olds aren’t immune; a single case study in 2024 showed a 42‑year‑old teacher develop severe keratitis after shingles.
Early Signs of Ocular Shingles
Detecting the problem early is the single biggest factor in preserving sight. Look for the following symptoms, usually appearing within a few days of the skin rash:
- Burning or itching around the eye, often before the rash shows.
- A painful, grouped vesicular rash on the forehead, scalp, or eyelid - the classic “shingles band.”
- Redness of the white part of the eye (conjunctival injection).
- Blurred or double vision, especially if the cornea is involved.
- Light sensitivity (photophobia) and excessive tearing.
If you notice any of these, treat it as an emergency-time is vision.
Protecting Your Vision: Prevention First
The most effective guard against eye‑shingles is vaccination.
- Shingles vaccine (Recombinant Zoster Vaccine, Shingrix) - recommended for adults 50+ and immunocompromised patients. Clinical trials in 2023 showed a 90% reduction in shingles overall and a 70% drop in ophthalmic involvement.
- Maintain a healthy immune system: balanced nutrition, regular exercise, adequate sleep, and stress management.
- Avoid known triggers such as prolonged sun exposure without UV protection, which can weaken corneal defenses.
Even after vaccination, breakthrough cases can happen, so stay vigilant.
Treatment Options When the Eye Is Involved
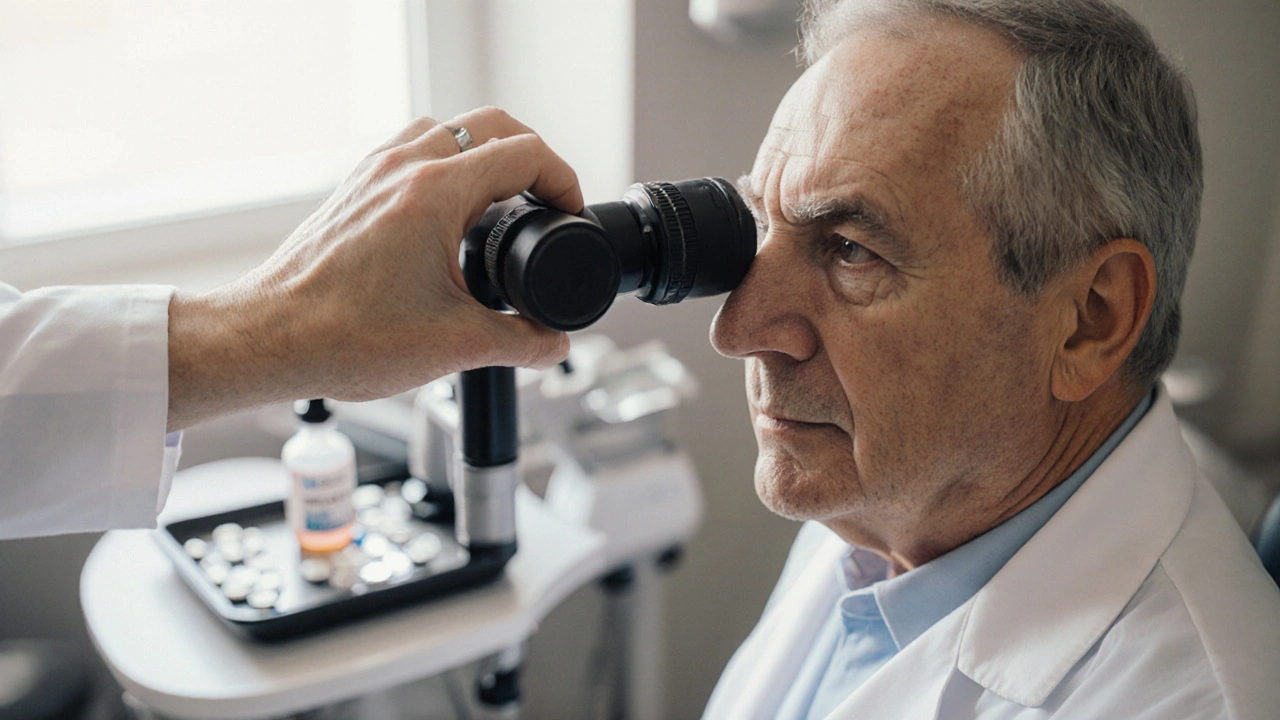
Once herpes zoster ophthalmicus is diagnosed, coordinated care between a primary doctor and an Ophthalmologist a medical specialist who treats eye diseases is essential.
Antiviral Medication
High‑dose Antiviral medication such as oral acyclovir, valacyclovir, or famciclovir should start within 72hours of rash onset. Typical regimens:
- Valacyclovir 1g three times daily for 7days.
- Acyclovir 800mg five times daily for 7days.
These drugs limit viral replication, reduce inflammation, and cut the risk of corneal scarring by about 50%.
Eye‑Drop Therapy
Topical steroids (e.g., prednisolone acetate) control severe inflammation but must be balanced against the risk of increased intra‑ocular pressure. Typically, an ophthalmologist prescribes a tapering schedule over 2-4weeks.
Artificial tears and lubricating ointments keep the surface moist, especially if a corneal ulcer forms.
Adjunct Treatments
- Oral analgesics for pain control (ibuprofen or acetaminophen).
- Topical antibiotics if a secondary bacterial infection is suspected.
- Protective eye patches at night to reduce exposure and aid healing.
Close follow‑up-often daily for the first week-allows the specialist to adjust drops and catch complications early.
Managing Aftereffects and When to Seek Help
Even with prompt treatment, some patients develop lingering issues:
- Post‑herpetic neuralgia - chronic eye‑area pain lasting months.
- Corneal scarring - may need a laser procedure or corneal transplant.
- Glaucoma - steroid‑induced pressure spikes require medication.
If vision worsens, you notice new floaters, or eye pressure feels “tight,” schedule an urgent retinal exam.

Quick Reference Checklist
- Know the vaccine schedule - two doses, 2‑6months apart.
- Watch for forehead/eyelid rash plus eye pain.
- Seek care within 72hours for antivirals.
- Follow ophthalmologist‑prescribed eye‑drop regimen.
- Attend all follow‑up visits; report any vision change immediately.
Comparison of Common Ocular Shingles Complications
| Complication | Typical Symptom | Risk of Vision Loss | Primary Treatment |
|---|---|---|---|
| Conjunctivitis | Red, gritty eye | Low | Lubricants + antivirals |
| Keratitis | Pain, blurry vision, corneal ulcer | Medium‑High | Antivirals + steroid drops |
| Uveitis | Photophobia, eye redness, floaters | Medium | Systemic steroids + antivirals |
| Retinitis | Sudden vision loss, scotomas | Very High | High‑dose IV antivirals + close monitoring |
Frequently Asked Questions
Can shingles affect only one eye?
Yes. Herpes zoster ophthalmicus usually involves the eye on the same side as the skin rash. Bilateral involvement is rare but can occur in severely immunocompromised patients.
Is the Shingrix vaccine safe for people with eye disease?
Clinical data up to 2024 show no increase in ocular side effects. The vaccine is recommended for anyone over 50, even if they have glaucoma or dry‑eye syndrome.
What if I miss the 72‑hour window for antivirals?
Treatment can still help, but the benefit diminishes. Oral antivirals are still given, and the ophthalmologist may add stronger topical therapy or consider intravenous meds in severe cases.
Can steroids cause more infection?
When used under specialist supervision, the anti‑inflammatory benefit outweighs the infection risk. Steroids are tapered quickly and combined with antivirals to keep the virus in check.
How long does vision recovery take?
Mild cases often improve within 2‑4weeks. More severe keratitis or uveitis may need 3‑6months, and scarring can require surgical correction to restore vision.
Bottom line: shingles can threaten your sight, but early vaccination, rapid antiviral therapy, and close eye‑care follow‑up keep the odds of permanent damage low. Stay alert, protect your immune health, and don’t wait to see an eye doctor if symptoms appear.
Comments
mathokozo mbuzi October 6, 2025 at 17:46
Ocular involvement in herpes zoster represents a clear reminder that viral reactivation can extend beyond cutaneous manifestations; early antiviral therapy remains the cornerstone of preventing irreversible damage. The ophthalmic branch of the trigeminal nerve offers a direct conduit to the cornea and retina, making prompt recognition vital. Patients over the age of 60, as well as those with compromised immunity, should be educated about the characteristic periorbital rash and associated photophobia. Moreover, integrating the Shingrix vaccine into routine preventive care can substantially lower the incidence of such complications. Vigilant monitoring for red eye, pain, or visual disturbances within the first 72 hours can facilitate timely specialist referral.
Penny X October 7, 2025 at 13:12
It is a moral imperative to confront the scourge of ocular shingles with unwavering resolve; the evidence unequivocally demonstrates that vaccination is not merely optional but ethically obligatory. One must denounce any complacency that permits preventable vision loss to persist in our communities. The clinical data cited herein-highlighting a 70% reduction in ophthalmic involvement-mandates immediate public health action. Let us, therefore, champion widespread immunization with the gravitas it deserves.
Amy Aims October 8, 2025 at 08:39
Great job laying out the steps, this really helped me understand why early treatment matters! 😊 If anyone’s unsure about the vaccine schedule, just remember it’s two doses, a few months apart, and it can save your sight. Stay positive and keep those eyes protected! 🌟
Shaik Basha October 9, 2025 at 04:06
Yo, this guide is super helpful, but lemme add a lil tip-if you get that itchy tinglin’ feeling around your eye, don’t wait for the rash to fully show up. Grab a doc ASAP, because those antivirals work best before the pain peaks. Also, wear sunglasses even if it’s cloudy, it helps protect the cornea from UV‑induced stress. Stay chill and keep that vision sharp!
Michael Ieradi October 9, 2025 at 23:32
Vaccination is essential.
Stephanie Zuidervliet October 10, 2025 at 18:59
Honestly, the article over‑hypes the vaccine-sure, it’s good, but you’re not going to become immortal overnight!!! The real issue is that many people ignore the early signs until it’s too late, and that’s where the tragedy lies… we need more education, not just a glossy vaccine endorsement!!!
Dawn Mich October 11, 2025 at 14:26
The pharma conglomerates don’t want you to know the truth about these so‑called “vaccines.” They’re pushing a narrative that masks a deeper agenda of control, and the rapid rollout sidesteps thorough long‑term studies. Keep your eyes open, question the data, and consider the hidden risks that mainstream sources conveniently ignore.
Eric Sevigny October 12, 2025 at 09:52
While the article is comprehensive, a few practical points merit emphasis: first, ensure that patients with a history of ocular disease receive baseline visual acuity testing before initiating antivirals. Second, consider adjunctive oral steroids only under ophthalmic supervision to mitigate inflammation without compromising viral clearance. Lastly, educate patients on proper eye‑drop instillation techniques to maximize therapeutic benefit. These nuances can improve outcomes significantly.
Glenda Rosa October 13, 2025 at 05:19
Ah, the classic over‑reliance on vaccination as a panacea-quite the melodramatic chorus, isn’t it? While immunization is a heavyweight champion, one must not discount the sheer power of lifestyle fortification: nutrition, stress reduction, and robust sleep hygiene act as silent guardians against viral resurgence. Let’s not surrender nuance to the singular, glorified narrative of a needle.
charlise webster October 14, 2025 at 00:46
Interesting take, though I’d argue that the data on vaccine efficacy against ocular shingles, while promising, still leaves room for debate. Some studies suggest variable protection across age brackets, and real‑world adherence to the two‑dose schedule is far from perfect. A balanced view should weigh these uncertainties.
lata Kide October 14, 2025 at 20:12
Wow, the article really hits the nail on the head! 😱 But remember, folks-if you feel any tingling around the eyes, act fast! 🌈💪 Stay safe and don’t let shingles steal your sparkle! ✨👁️🗨️
Mark Eddinger October 15, 2025 at 15:39
I concur with the points raised by the previous contributor regarding baseline assessments; ensuring a thorough ophthalmic work‑up before antiviral initiation can indeed preempt complications. Additionally, reinforcing patient education on the urgency of seeking care within the 72‑hour window is paramount for optimal outcomes.
Francisco Garcia October 16, 2025 at 11:06
Your emphasis on baseline testing is spot‑on, and it dovetails nicely with community outreach programs that aim to raise awareness among at‑risk populations. Moreover, integrating tele‑ophthalmology consultations could bridge the gap for patients living in remote areas, ensuring timely specialist input. It would be beneficial to develop standardized checklists that primary care providers can use to flag potential ocular involvement early on.
Patrick Renneker October 17, 2025 at 06:32
While the preceding remarks laud the virtues of prompt ophthalmic evaluation, they inadvertently sidestep a critical dimension: the pharmacoeconomic ramifications of indiscriminate antiviral deployment. It is not enough to champion early treatment without scrutinizing the cost‑effectiveness of deploying high‑dose valacyclovir across a broad demographic, especially when the incidence of severe ocular sequelae remains relatively low. Moreover, the reliance on a two‑dose vaccine regimen presupposes impeccable adherence-a scenario seldom realized in real‑world settings where socioeconomic barriers impede full immunization. One must also consider the emergent reports of rare but serious adverse events associated with the recombinant zoster vaccine, which, while statistically marginal, nonetheless warrant vigilant post‑marketing surveillance. The narrative that vaccination uniformly reduces ophthalmic complications fails to acknowledge the heterogeneity of immune responses among immunosenescent individuals; certain cohorts may derive negligible benefit, thereby questioning the blanket recommendation. Furthermore, the emphasis on antiviral therapy within the 72‑hour window, though evidence‑based, does not address the logistical challenges faced by patients residing in underserved regions lacking immediate access to ophthalmologists. Telemedicine, while promising, cannot substitute for the nuanced slit‑lamp examination required to detect subtle corneal infiltrates. In addition, the literature cited in the source material often derives from controlled clinical trials with stringent inclusion criteria, rendering extrapolation to the general population fraught with uncertainty. Health policymakers, therefore, must weigh the incremental benefit of mass vaccination against the opportunity costs of allocating resources away from other pressing public health priorities. Lastly, fostering a culture of vaccine complacency could engender a false sense of security, leading individuals to neglect other preventive measures such as UV protection and systemic health optimization. In sum, a more balanced discourse that incorporates cost‑benefit analyses, real‑world adherence data, and a critical appraisal of adverse event profiles is indispensable for formulating sound clinical guidelines.
Nathan Squire October 18, 2025 at 01:59
Ah, the classic conspiracy riff-amusing, but let’s not let paranoia eclipse the solid evidence supporting vaccine efficacy. While vigilance is healthy, dismissing the consensus of peer‑reviewed studies does a disservice to those at genuine risk of ocular complications.
Sean Kemmis October 18, 2025 at 21:26
The previous commentary portrays the vaccine in an unrealistically rosy light; a more critical lens reveals that the post‑marketing surveillance data still show sporadic instances of severe ocular inflammation potentially linked to immunization. Ignoring these outliers does not constitute balanced analysis.