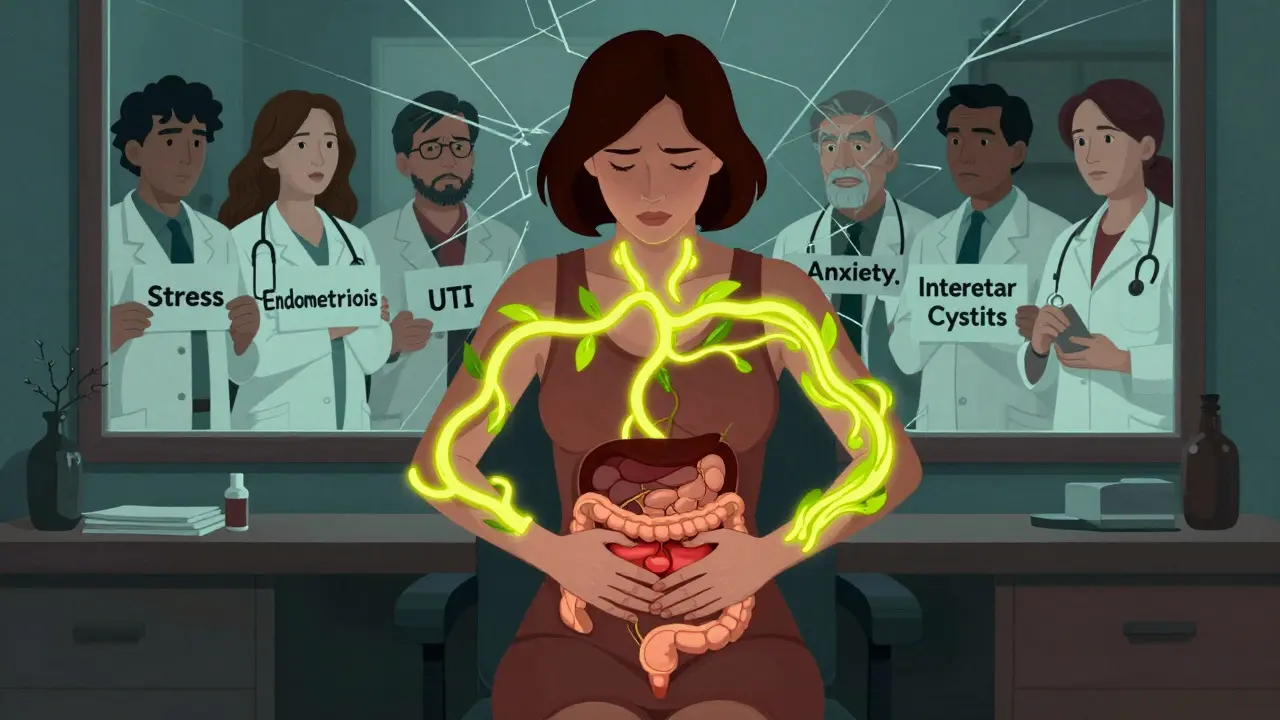
Why Pelvic Pain in Women Is So Often Misdiagnosed
Imagine feeling constant pain in your lower belly, needing to pee every hour, and wincing during sex - all while doctors tell you it’s just stress, or you’re imagining it. For millions of women, this isn’t a rare nightmare. It’s daily life. Two conditions - endometriosis and interstitial cystitis - are behind much of this suffering, and they look so similar that even experienced doctors mix them up. The result? Years lost to wrong treatments, unnecessary antibiotics, and emotional burnout.
Endometriosis happens when tissue like the lining of the uterus grows outside the womb - on the ovaries, bowel, bladder, or even the diaphragm. It’s not just heavy periods. It’s sharp, stabbing pain that spikes around your cycle, sometimes so bad you can’t walk. Interstitial cystitis (IC), on the other hand, is a bladder condition that causes chronic pain, urgency, and frequency without infection. The bladder wall becomes inflamed, and even small amounts of urine feel like pressure on fire.
Here’s the kicker: 65% of women with chronic pelvic pain have both conditions at the same time, according to a major 2011 study of 178 patients. Yet most doctors still look for one or the other. That’s like searching for one leak in a boat with two holes. The longer you wait, the worse it gets. On average, women wait 7 to 10 years to get a correct endometriosis diagnosis. For IC, it’s still 3 to 5 years. That’s not bad luck - it’s a system failure.
How to Tell the Difference - When Symptoms Overlap
At first glance, endometriosis and IC sound almost identical. Both cause pelvic pain, frequent urination, pain during sex, and discomfort when the bladder fills. But the clues are there if you know where to look.
Endometriosis pain usually follows your menstrual cycle. If your pain gets worse just before or during your period, it’s a strong sign. Around 92% of women with endometriosis report cyclical pain. You might also notice pain during bowel movements, especially during your period, or even coughing or sneezing if the tissue is near the diaphragm. Some women even cough up blood during their period - yes, really - if endometriosis affects the lungs.
IC pain, by contrast, doesn’t care about your cycle. It’s steady. It flares up after eating spicy food, drinking coffee, or sitting too long. But it doesn’t spike with your period like endometriosis does. Only about 45% of IC patients notice worse symptoms around their cycle. The biggest red flag for IC? Pain when your bladder is full, and relief after peeing. You might go 15 times a day, sometimes only a few drops at a time. And unlike endometriosis, IC rarely causes bleeding - unless the endometriosis has spread to the bladder wall.
That’s the twist: if you have endometriosis on your bladder (which happens in 1-12% of cases), you can get blood in your urine. That’s rare in pure IC. If you see pink or red in your urine, especially around your period, it’s a signal to dig deeper.
The Diagnosis Trap: Why Tests Often Fail
Here’s where things get messy. There’s no blood test for endometriosis. No scan can catch it unless it’s deep and large. The only way to confirm it? Surgery. Laparoscopy - a small camera inserted into the abdomen - is the gold standard. Surgeons look for lesions, then cut them out and send them to a lab. This isn’t a quick office visit. It costs $5,000 to $15,000 in the U.S., takes weeks to recover from, and requires a surgeon trained in deep excision. Only 15% of OB/GYNs in the U.S. have that skill.
IC is even trickier. There’s no definitive test. Diagnosis means ruling everything else out. You need negative urine cultures, negative STI tests, and a cystoscopy - where a scope checks your bladder lining. A Potassium Sensitivity Test (PST) might be done: if your bladder hurts badly when potassium solution is introduced, it suggests IC. But this test misses 20% of cases. And if you have endometriosis on your bladder, the PST might be positive anyway - even if you don’t have classic IC.
Many women are told they have recurrent UTIs. In fact, 63% of IC patients were misdiagnosed this way before getting the right answer. Antibiotics didn’t help because there was no infection. That’s medical gaslighting - and it’s common. One survey found 76% of IC patients were told their pain was “all in their head.”
What Happens When You Get Both - And How to Treat Them
When endometriosis and IC show up together, it’s not just double the pain. It’s a cycle. Endometriosis causes inflammation and scar tissue. That scar tissue pulls on nerves and muscles, leading to pelvic floor spasms. Those spasms make the bladder feel like it’s constantly full - triggering IC symptoms. So you don’t just have two separate problems. You have one tangled mess.
That’s why treating just one condition often fails. If you have IC and get bladder treatments like dietary changes, bladder instillations, or oral meds like Elmiron - but still have endometriosis on your bladder wall - your symptoms won’t improve. A 2022 review of 342 patients showed 63% had major relief only after both conditions were treated.
For endometriosis, excision surgery is the most effective fix. Removing lesions - not just burning them - gives the best long-term results. For IC, a mix of approaches works: avoiding trigger foods (citrus, caffeine, alcohol), pelvic floor physical therapy, and sometimes medications like pentosan polysulfate sodium. But if endometriosis is still there, none of it sticks.
One woman, u/BladderWarrior on Reddit, had seven years of IC diagnosis before her third laparoscopy found endometriosis on her bladder wall. After surgery, her urinary symptoms dropped by 80%. That’s not a fluke. It’s the pattern.
Who’s Getting Left Behind - And Why
This isn’t just about misdiagnosis. It’s about who gets ignored. Black women wait nearly four years longer than white women to get diagnosed with endometriosis. Rural women have fewer specialists nearby. Low-income women get denied insurance for cystoscopies or laparoscopies - 44% report initial denials. Primary care doctors rarely screen for pelvic floor dysfunction, even though 92% of women with either condition have it.
And the specialists? There are only about 350 board-certified urogynecologists in the entire U.S. Most women never see one. The system is built for single-diagnosis thinking. But the science says: pelvic pain is rarely one thing.
That’s why new guidelines from the International Pelvic Pain Society now recommend that every woman with chronic pelvic pain gets evaluated by both a gynecologist trained in endometriosis excision AND a urologist or urogynecologist - at the same time. No more waiting. No more guessing.

What You Can Do Right Now
If you’re suffering, here’s what to do:
- Track your symptoms for at least one full menstrual cycle. Note when pain happens, what triggers it, and if you see blood in your urine.
- Ask for a voiding diary - write down every time you pee, how much, and how much pain you feel. This is a powerful diagnostic tool.
- Request a pelvic exam that includes checking for pelvic floor muscle tension. Tight muscles can mimic IC.
- Insist on ruling out endometriosis before accepting an IC diagnosis. If your doctor says, “We’ll treat it as IC,” push back. Say: “I want to be checked for endometriosis too.”
- Find a specialist. Look for surgeons who specialize in deep excision of endometriosis - not ablation. Search the Endometriosis Foundation’s directory or ask for referrals from pelvic pain support groups.
Don’t wait for a perfect test. Your pain is real. And you deserve a diagnosis that sees the whole picture - not just the part that fits a checklist.
What’s Changing - And Why There’s Hope
In early 2024, the NIH gave $4.2 million to the University of Michigan to find biomarkers that can tell endometriosis and IC apart with a simple blood or urine test. That’s huge. Right now, we’re stuck with invasive procedures. In five years, that could change.
The Endometriosis Foundation updated its surgical guidelines in January 2024 to require bladder evaluation during every endometriosis surgery. That means more women will get diagnosed early - before IC becomes a secondary problem.
And the conversation is shifting. Doctors are finally admitting that IC might not be its own disease - but often a symptom of something else, like endometriosis or pelvic floor dysfunction. That’s not giving up on IC - it’s understanding it better.
The future isn’t about choosing one diagnosis. It’s about seeing pelvic pain as a network - where organs, nerves, and muscles talk to each other. When you fix one part, the whole system heals.
Can endometriosis cause symptoms that look like interstitial cystitis?
Yes. Endometriosis can grow on or near the bladder, causing urinary urgency, frequency, and pain - all classic IC symptoms. In fact, up to 12% of endometriosis patients have bladder involvement. Many women are misdiagnosed with IC when the real issue is endometriosis on the bladder wall. This is why experts now recommend evaluating for endometriosis before confirming an IC diagnosis.
Is there a blood test for endometriosis or interstitial cystitis?
No. There are currently no approved blood or urine tests that can definitively diagnose either condition. Endometriosis requires surgical confirmation via laparoscopy and biopsy. IC is diagnosed by ruling out other causes and using clinical criteria like the PUF scale or potassium sensitivity test. Researchers are working on biomarkers, but none are available for clinical use yet.
Why do so many women get misdiagnosed with UTIs?
Because urinary urgency, frequency, and pain are common in both IC and endometriosis with bladder involvement. Doctors often assume these are signs of infection and prescribe antibiotics. But if there’s no bacteria in the urine - which is true in 90% of IC cases and many endometriosis cases - antibiotics won’t help. Studies show 63% of IC patients were treated for UTIs multiple times before getting the right diagnosis.
Can pelvic floor physical therapy help with both conditions?
Yes. Pelvic floor dysfunction is present in 92% of women with either endometriosis or IC. Tight, overactive pelvic muscles can cause or worsen pain, urgency, and discomfort. Physical therapy that includes manual release, biofeedback, and relaxation techniques can significantly reduce symptoms - even when the root cause is endometriosis. It’s not a cure, but it’s a critical part of recovery.
Should I get surgery if I think I have endometriosis?
If your symptoms are severe, persistent, and not improving with medication or lifestyle changes, yes - especially if you suspect endometriosis. Laparoscopic excision surgery is the only way to confirm the diagnosis and remove lesions. Ablation (burning) is less effective. Look for a surgeon trained in deep excision who will remove tissue completely, not just surface lesions. Surgery often improves both pelvic pain and urinary symptoms - even if IC is also present.
Comments
Mike Rose January 30, 2026 at 17:18
lol so basically doctors are just dumb and women are too weak to deal with pain? got it.
Russ Kelemen January 31, 2026 at 01:05
This is one of those rare posts that doesn't just list symptoms but actually tries to connect the dots. Too many people treat pain like it's a puzzle with one piece. The body doesn't work like that. It's a web. When one thread pulls, everything else tenses up. That's why treating just one condition often fails. You're not just fixing a bladder or removing tissue-you're unraveling a knot that's been tightening for years.
April Allen January 31, 2026 at 17:34
The overlap between endometriosis and IC is clinically significant, particularly in the context of neurogenic inflammation and central sensitization. Bladder wall infiltration by endometrial implants can trigger mast cell degranulation and afferent nerve hypersensitivity, which mimics IC pathophysiology. This is why empirical IC treatment without laparoscopic evaluation is often futile. The 2022 cohort study cited demonstrates that dual-pathway intervention yields superior outcomes in 63% of comorbid cases. Clinicians must adopt a systems-based diagnostic algorithm rather than a siloed approach.
Kathleen Riley February 1, 2026 at 04:35
It is imperative to acknowledge the systemic epistemological failure inherent in contemporary gynecological practice. The reductionist paradigm, predicated upon discrete pathological entities, fails to account for the phenomenological complexity of chronic pelvic pain. The conflation of symptomatology with diagnostic certainty constitutes a form of medical hermeneutic negligence.
Sazzy De February 3, 2026 at 03:47
I had both and no one believed me for 6 years. Just keep track of your stuff and find someone who actually listens. It’s not magic, just patience and persistence
Jodi Olson February 4, 2026 at 14:12
The real issue isn't the misdiagnosis it's that we're taught to endure pain as women. You're not broken. The system is. And if your doctor won't look deeper, find someone who will. Your pain is data not drama
Carolyn Whitehead February 4, 2026 at 22:44
you're not alone and you're not crazy. i went through this too and finding the right person made all the difference. just keep going
Beth Beltway February 5, 2026 at 23:57
People who don't get surgery are just giving up. If you're still having symptoms after 2 years of 'lifestyle changes' you're either lazy or you're in denial. This isn't about being a victim. It's about taking control. Stop blaming doctors and start demanding answers.
kate jones February 7, 2026 at 16:17
The integration of pelvic floor physical therapy as a co-intervention is not ancillary-it is foundational. Pelvic floor hypertonicity is a secondary adaptive response to chronic nociceptive input from endometriotic lesions or bladder inflammation. Manual therapy, neuromuscular re-education, and biofeedback modulate central sensitization and reduce referred pain patterns. This is evidence-based, not complementary. It must be included in first-line multimodal care protocols.
Kimberly Reker February 7, 2026 at 18:29
i wish i knew all this 10 years ago. the moment i found a surgeon who did excision instead of burning? my life changed. don't settle for 'maybe it's stress'. you deserve better. you're not overreacting. you're just finally being heard