When your bones start to weaken without warning, even a simple stumble can lead to a break. That’s the reality for millions with osteoporosis, a silent disease where bone tissue thins over time, turning once-strong skeletons into fragile structures. It’s not just about aging - it’s about how fast your body loses bone compared to how well it rebuilds it. By age 65, nearly half of all women and a quarter of men will have low bone density serious enough to be called osteoporosis. And while it doesn’t hurt until something breaks, the damage is already done long before the fall.
What Exactly Is Osteoporosis?
Osteoporosis isn’t just "brittle bones." It’s a measurable disease defined by low bone mineral density and changes in bone structure that make fractures far more likely. The World Health Organization set the standard in 1994: if your bone density is 2.5 standard deviations below the average of a healthy young adult, you have osteoporosis. That’s not a guess - it’s a scan. A DXA scan, done in minutes, can show exactly how much bone you’ve lost.
Why does this happen? For women, it’s often tied to menopause. Estrogen drops sharply after menopause, and that hormone plays a key role in keeping bone cells called osteoclasts in check. Without it, bone breaks down faster than it’s replaced. Men lose bone too, but slower - and usually later. Other factors like long-term steroid use, smoking, low vitamin D, and even certain cancers can speed up the process.
The real danger? Fractures. Not the kind from car crashes or sports. These are fragility fractures - from a fall from standing height, or even just bending over. Hip fractures are the most feared. About 20% of people who suffer one die within a year. Many never walk without help again. Spine fractures can cause you to shrink in height, develop a hunched back, or feel constant pain. And here’s the kicker: most people don’t know they have osteoporosis until they break a bone.
How Bisphosphonates Work to Stop Bone Loss
For over 30 years, bisphosphonates have been the go-to treatment for osteoporosis. These aren’t miracle drugs that rebuild bone - they’re bone protectors. They work by slowing down osteoclasts, the cells that chew away old bone. Think of it like hitting pause on the demolition crew so the construction crew (osteoblasts) can catch up.
There are two main types: non-nitrogen and nitrogen-containing. The nitrogen ones - like alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast) - are stronger and used first. They block a key enzyme in osteoclasts called farnesyl pyrophosphate synthase. Without it, the cells can’t function properly and eventually die. That means less bone breakdown, more density over time.
Studies show these drugs cut fracture risk dramatically. Alendronate reduces spine fractures by 48% and hip fractures by 51% over three years. Zoledronic acid, given as a yearly IV infusion, cuts hip fractures by 41% in high-risk patients. That’s not small. That’s life-changing.
Oral vs. IV: Which One Is Right for You?
Bisphosphonates come in two forms: pills and shots. Oral versions are cheaper and easier to get, but they’re picky. You have to take them first thing in the morning, on an empty stomach, with a full glass of water. Then you must stay upright for at least 30 minutes - no lying down, no bending over, no eating. Miss a step, and the pill can burn your esophagus. That’s why nearly half of people stop taking them within a year.
For those who can’t tolerate the pills, or just forget them, zoledronic acid is a game-changer. It’s given once a year through an IV, usually in a doctor’s office. No daily reminders. No stomach upset. Side effects are usually mild - flu-like symptoms for a day or two after the infusion. Many patients switch to this after trying oral versions and finding them too harsh.
But even IV bisphosphonates aren’t perfect. They’re not for people with poor kidney function. Your creatinine clearance must be above 35 mL/min. And if you’ve had dental work done recently, your doctor will likely delay treatment - there’s a rare but serious risk of jawbone death, called osteonecrosis, especially after major dental procedures.
Side Effects and Long-Term Risks
Most people tolerate bisphosphonates well. But some side effects are common enough to matter. Up to 15% of people on oral versions get heartburn, nausea, or stomach pain. Rarely, the esophagus gets inflamed. That’s why you need to follow the dosing rules exactly.
Then there are the rare but serious risks. Atypical femoral fractures - cracks in the thigh bone that happen without trauma - occur in about 3 to 5 cases per 10,000 patient-years. It sounds low, but if you’ve been on bisphosphonates for more than five years, your doctor will watch for thigh or groin pain. Osteonecrosis of the jaw is even rarer - about 1 in 2,500 to 1 in 10,000 patients - but it’s devastating. That’s why dentists and doctors now talk before you start treatment. Clean teeth. No extractions until after you’ve been on the drug for a while.
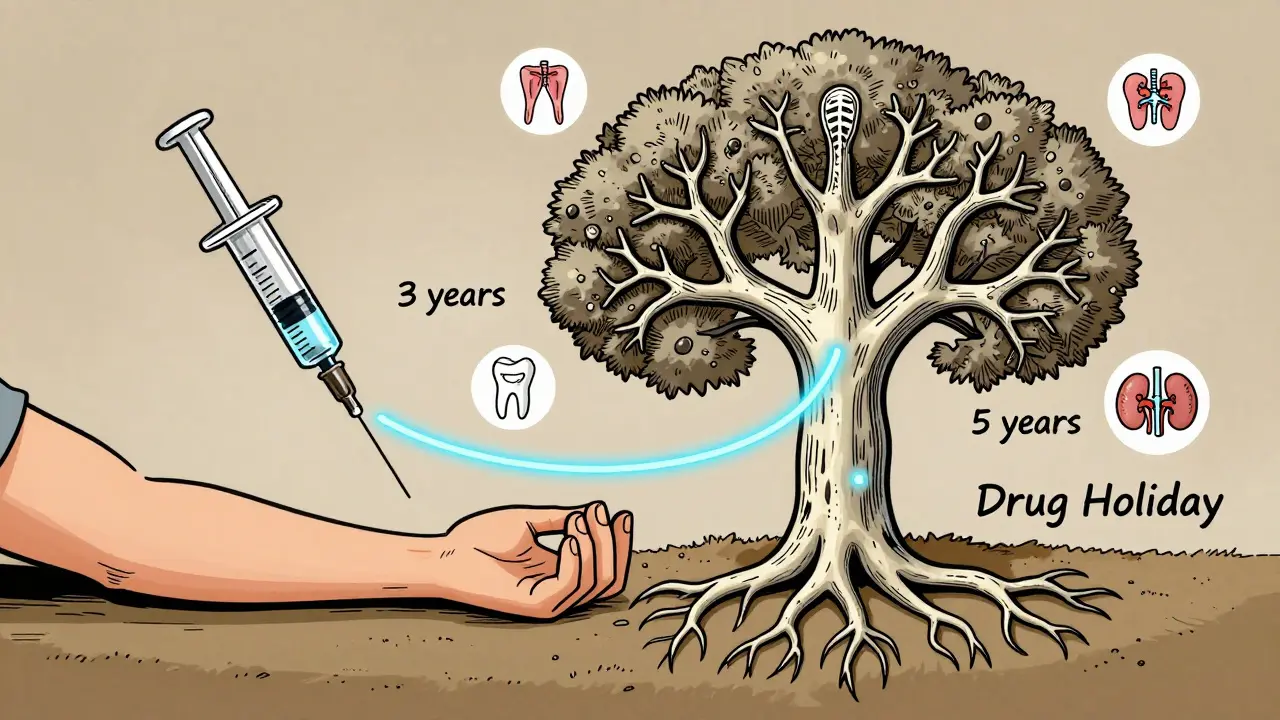
And here’s what many don’t know: bisphosphonates can stay in your bones for years after you stop. That’s why doctors now recommend a "drug holiday." If you’re low-risk - no prior fractures, good bone density after 3-5 years - you might pause the meds for a year or two. Your bone density is still protected by the drug lingering in your skeleton. But if your risk goes up again - maybe you fall, or your bone density drops - you restart. It’s not one-size-fits-all. It’s personalized.
Bisphosphonates vs. Other Treatments
Bisphosphonates aren’t the only option. But they’re still the most used - about 65% of prescriptions in the U.S. go to them. Why? Cost, safety, and proof.
Denosumab (Prolia) is a strong competitor. It’s a monthly or six-monthly injection that blocks a different pathway in bone breakdown. It can improve bone density even more than bisphosphonates. But here’s the catch: if you stop it, your bone density plummets fast. Some people have had multiple spine fractures within months of missing a dose. That means you can’t just quit it. You’re locked in.
Teriparatide (Forteo) does the opposite - it builds bone. It’s a synthetic form of parathyroid hormone that tells your body to make new bone. It works well, boosting density by 9-13% over 18 months. But it’s expensive - over $1,800 a month - and you can only use it for two years. After that, you switch to something else, usually a bisphosphonate.
Then there’s romosozumab (Evenity). It’s newer, and it does two things at once: builds bone and slows breakdown. It cuts spine fractures by 73%. But it carries a black box warning for heart attack and stroke risk. So it’s only used in people with high fracture risk and no heart disease.
For most people, bisphosphonates still win. They’re cheaper, safer over the long term, and have been studied in hundreds of thousands of patients. They’re the foundation. Others are for special cases - when bisphosphonates fail, aren’t tolerated, or the risk is too high.
Who Should Be Tested and When to Start
Not everyone needs a bone scan. But if you’re a woman over 65, or a man over 70, get one. If you’re younger but had a fracture from a minor fall, have a family history of hip fractures, take steroids for more than three months, or have rheumatoid arthritis - get tested. The Fracture Risk Assessment Tool (FRAX) helps doctors decide. It uses your age, weight, sex, smoking status, and history of fractures to calculate your 10-year risk. If your risk of a major fracture is over 20%, or your hip fracture risk is over 3%, treatment is recommended.
Before starting any medication, your doctor will check your kidney function, vitamin D levels, and calcium. You need enough of these for the drugs to work. Many people with osteoporosis are low on vitamin D - even in sunny places like Sydney. Fix that first.
What Patients Really Say
Online forums are full of stories. One woman in her 70s says alendronate kept her from breaking her other hip after the first one. Another says she switched from daily pills to yearly IVs because the stomach pain was unbearable. A man in his 60s stopped after five years because his doctor said he was low-risk now. He’s still monitoring his bone density every two years.
But many quit because of the hassle. Taking a pill first thing in the morning, staying upright, waiting an hour before breakfast - it’s hard to stick to. That’s why adherence is only 50-70% after one year. Doctors now spend more time explaining how to take the pills correctly. Some even give patients a checklist. A simple reminder can make all the difference.
The Future of Osteoporosis Treatment
Research is moving fast. The 2023 DATA-HD study showed that after 10 years of combining teriparatide and alendronate, patients still had strong bones. That challenges the old idea that you can’t use these drugs for long. We’re also learning more about who benefits most from drug holidays and who should stay on treatment. Biomarkers to track bone turnover are being tested - maybe one day we’ll know exactly when to pause or restart based on a blood test.
But for now, bisphosphonates remain the backbone of treatment. They’re not flashy. They don’t rebuild bone like anabolic drugs. But they stop the loss. And for most people, that’s enough. Preventing one hip fracture saves thousands in hospital costs and years of lost independence. That’s why they’re still the first choice - and likely to stay that way.

Comments
Lauren Wall January 21, 2026 at 07:24
My grandma broke her hip at 72 just from stepping off a curb. No one told her she had osteoporosis until it was too late. Why aren't we screening everyone over 60? It's not rocket science.
Kenji Gaerlan January 22, 2026 at 01:44
so like… bisphosphonates are just like… bone freeze rays? lol i took fosamax once and felt like i was dying for 3 days. no thanks. 🤮
arun mehta January 23, 2026 at 09:45
Thank you for this detailed and compassionate breakdown. 💪 In India, many elderly don’t even get basic calcium supplements, let alone DXA scans. Education and access are the real challenges here. Let’s not forget that medicine is only as good as its reach. 🌏❤️
Chiraghuddin Qureshi January 24, 2026 at 14:06
From Delhi to Detroit - this hits home. My uncle in Jaipur used to walk 5km daily until he fractured his spine. No scans, no meds, just prayer and painkillers. We need global awareness, not just Western protocols. 🙏🫶
Margaret Khaemba January 25, 2026 at 06:12
Wait - so if you stop bisphosphonates, does your bone density just drop back down? I thought once you built it up, it stayed? Also, anyone else find the ‘drug holiday’ idea weird? Like… taking a break from your bone armor?
Malik Ronquillo January 26, 2026 at 05:48
so you're telling me i gotta sit upright for 30 mins after a pill like i'm in a yoga class?? and if i slouch i get esophagus burns?? bro that's not medicine that's a punishment
and now they want me to pay $1800 a month for a drug that makes me feel like i got hit by a truck??
Brenda King January 26, 2026 at 17:59
I switched to the yearly IV after 2 years of oral meds and my stomach finally stopped screaming. I still take my vitamin D and walk every morning. It’s not just about the pill - it’s about the habit. You gotta move. You gotta eat. You gotta care. 💪
Keith Helm January 26, 2026 at 18:36
While the pharmacological mechanisms are well-documented, the adherence rates cited are concerning. A 50–70% discontinuation rate within one year suggests systemic failures in patient education and behavioral support infrastructure. This is not a medication issue; it is a healthcare delivery failure.
Daphne Mallari - Tolentino January 27, 2026 at 17:57
How quaint. You refer to this as ‘the backbone’ of treatment, as if it were some noble, time-tested pillar of medical wisdom. In reality, it’s the default option because it’s cheap, not because it’s optimal. The real innovation lies in anabolic agents - but of course, the insurance companies won’t cover them unless you’re literally dying on the floor.
Neil Ellis January 28, 2026 at 07:11
Imagine your bones as a crumbling castle. Bisphosphonates aren’t the builders - they’re the guards who stop the vandals from tearing down the walls. It’s not glamorous, but without them? The whole thing collapses. And honestly? Sometimes being the quiet hero is better than being the flashy one who burns out in two years. 🏰🛡️
Alec Amiri January 28, 2026 at 15:46
So let me get this straight - you take a drug that could give you a snapped femur from walking too hard, then you get jawbone death if you get a tooth pulled, and you're supposed to be grateful? This isn't medicine, it's Russian roulette with a prescription pad.
Lana Kabulova January 29, 2026 at 01:10
My mom’s on Prolia and they told her she can’t stop it or she’ll shatter like glass - so now she’s locked in for life. What if she gets sick? What if she can’t afford it? They don’t tell you the catch until it’s too late
Rob Sims January 29, 2026 at 01:49
Wow. So the solution to aging is just… poison your skeleton with a drug that lasts decades and might kill your jaw? And you call this progress? I’d rather just die falling than live like a walking pharmaceutical experiment.