Think you have allergies? Maybe you don’t. If you’re constantly sneezing, dripping, or stuffed up-but your allergy tests keep coming back negative-you might be dealing with nonallergic rhinitis. It’s not caused by pollen, dust mites, or pet dander. It’s triggered by things most people don’t even think of as problems: cold air, spicy food, perfume, or even a change in the weather. And it’s more common than you’d guess. Around 1 in 5 adults in Western countries live with it, and for many, it’s been going on for years without a proper diagnosis.
What Exactly Is Nonallergic Rhinitis?
Nonallergic rhinitis is chronic inflammation in your nose that isn’t caused by an immune reaction. Unlike allergic rhinitis, where your body overreacts to allergens by releasing histamine, this condition is about your nasal nerves going haywire. The autonomic nervous system-responsible for things like heart rate and digestion-loses its balance in the nasal passages. This leads to blood vessels swelling, mucus pouring out, and sneezing fits, all without any allergy involvement.
It’s not one thing. There are at least eight subtypes. The most common is vasomotor rhinitis, making up 60-70% of cases. Then there’s drug-induced rhinitis (from blood pressure meds like ACE inhibitors), hormonal rhinitis (common in pregnancy), gustatory rhinitis (triggered by eating), and occupational rhinitis (from workplace fumes or dust). Even aging plays a role-about 1 in 4 people over 70 develop senile rhinitis, where the nasal lining thins and becomes overly sensitive.
Doctors diagnose it by ruling everything else out. If your skin prick test is negative, your IgE levels are normal, and you’ve had symptoms for three months or more, it’s likely nonallergic rhinitis. Nasal smears often show neutrophils-not the eosinophils you’d see in allergies-which confirms it’s not an immune response.
What Triggers Your Nose? The Hidden Culprits
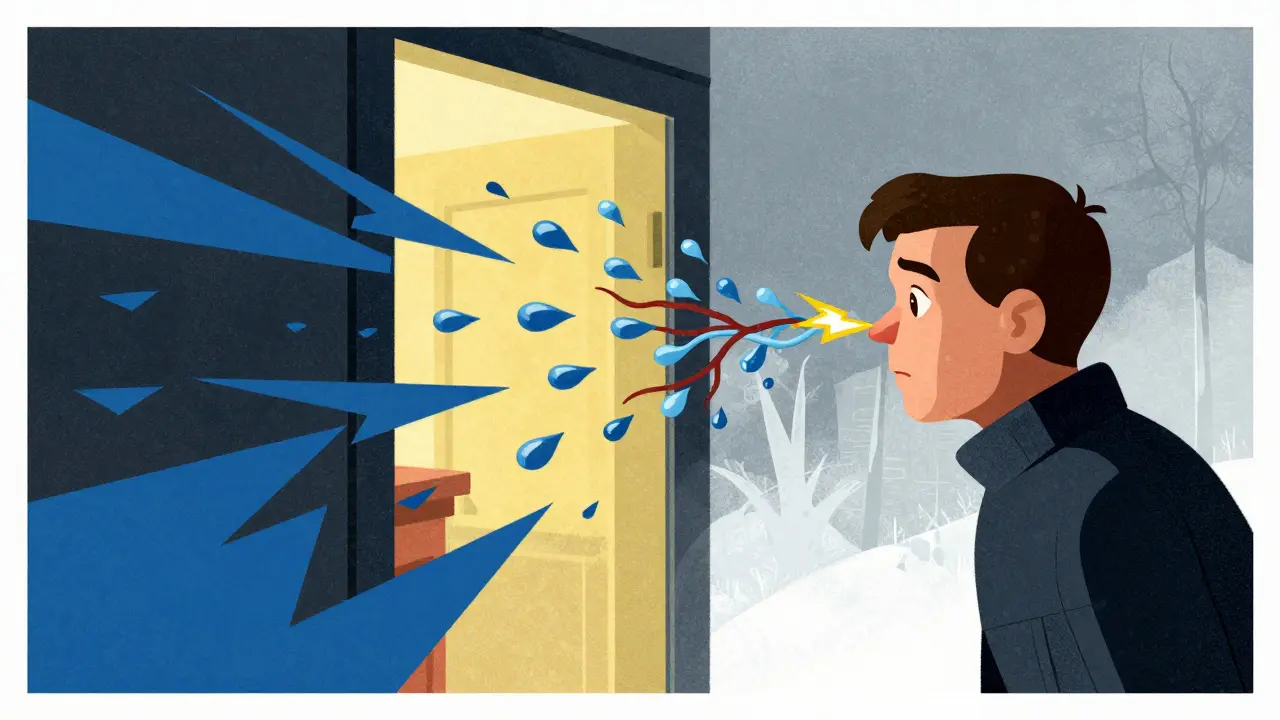
Here’s the tricky part: triggers aren’t always obvious. You might think it’s the cat, but it’s actually the new air freshener. Or you blame the cold, but it’s the 5°C drop in temperature that hits you when you walk out the door.
Environmental irritants are big ones. Tobacco smoke at just 0.05 mg/m³ can set off symptoms. Perfumes? You don’t need much-0.1 parts per million is enough. Paint fumes, cleaning products, and wildfire smoke (PM2.5 levels above 15 µg/m³) all act like lit matches to your nasal nerves. Even strong smells like garlic or incense can trigger a flood of mucus.
Weather changes are another silent enemy. A sudden drop in temperature, especially below 15°C, or a jump above 35°C, can cause immediate congestion. Humidity shifts of more than 20% in an hour? That’s enough. Barometric pressure changes as small as 5 mmHg can make your nose feel like it’s closing in. People in Sydney know this well-when the cold front rolls in from the south, nasal symptoms spike.
Food and drink are surprisingly common triggers. Spicy foods with capsaicin (think chili peppers, wasabi, hot curry) activate TRPV1 receptors in your nose-those same receptors that make you feel heat. Alcohol, even just a glass of wine, can cause runny nose in people with a blood alcohol level above 0.02%. And for many older adults, eating any meal-especially hot or greasy ones-triggers gustatory rhinitis. It’s not the food itself; it’s the steam, the smell, the temperature change.
Medications are often overlooked. About 1 in 5 people taking ACE inhibitors (like lisinopril) for high blood pressure develop nasal symptoms within weeks. Beta-blockers, NSAIDs like ibuprofen, and even hormone replacement therapy can do the same. And then there’s rhinitis medicamentosa-the rebound congestion from overusing nasal decongestant sprays. It’s a vicious cycle: spray to clear your nose, then need more because it gets worse.
How to Manage It-Without Allergy Meds
Since antihistamines don’t work well here (they target histamine, which isn’t the issue), treatment focuses on calming the nerves and blocking triggers.
Trigger avoidance is the first step-and it works. Studies show that using HEPA filters reduces symptoms by 35-40%. Cutting out strong perfumes, switching to fragrance-free products, and avoiding smoke can knock off 25-30% of flare-ups. For gustatory rhinitis, eating cooler meals or avoiding spicy foods cuts symptoms by 40-50%. Simple? Yes. Effective? Absolutely.
Nasal saline irrigation is the unsung hero. Rinsing your nose twice a day with isotonic (0.9%) or hypertonic (3%) salt water removes irritants, reduces swelling, and improves mucus flow. People who do this regularly report 60-70% symptom relief. It’s cheap, safe, and doesn’t interact with other meds. Just make sure you use distilled or boiled water-tap water can carry dangerous microbes.
Intranasal corticosteroids (like fluticasone) are the go-to for moderate to severe cases. They reduce inflammation in the nasal lining and cut symptoms by 50-60%. But they take time-2 to 4 weeks to kick in. Don’t give up after a few days. Side effects? Nosebleeds happen in 15-20% of users, but they’re usually mild.
Ipratropium bromide (Atrovent) is the only medication that specifically targets runny nose. It blocks the nerve signals that make mucus glands go wild. Within 48 hours, most users see a 70-80% drop in dripping. It doesn’t help with congestion, but if your main problem is a constant drip, this is the gold standard. The newer 0.03% formulation has fewer side effects and works just as well.
Azelastine nasal spray (an antihistamine) is sometimes used off-label. It helps about 30-40% of people, even though it’s not designed for nonallergic cases. The downside? A bitter taste in the mouth for 30-40% of users. It’s not first-line, but if other options fail, it’s worth a try.
What Doesn’t Work-and Why
Many people waste time and money on treatments that don’t help. Oral antihistamines like cetirizine or loratadine? They’re useless for nonallergic rhinitis. They block histamine, which isn’t driving the symptoms. Yet doctors still prescribe them because they’re familiar and easy to reach for.
Decongestant sprays like oxymetazoline (Afrin) give quick relief-but only for a few days. After that, your nose becomes dependent. You need more to get the same effect, then you get worse when you stop. This is rhinitis medicamentosa, and it’s a nightmare to reverse. The fix? Stop the spray cold turkey and use a nasal steroid for 7-10 days while your nose recovers. It works in 85-90% of cases, but it’s tough.
Immunotherapy (allergy shots) is also a dead end. If your tests are negative, shots won’t help. Yet 30-40% of people with nonallergic rhinitis are misdiagnosed and put on them anyway. That’s not just ineffective-it’s expensive and unnecessary.
Real People, Real Experiences
Online forums are full of stories. On Reddit, 78% of people with nonallergic rhinitis say they waited over three years to get diagnosed. Most were told they had allergies first. One woman in Melbourne spent five years on antihistamines before her ENT did a nasal smear and found neutrophils-not eosinophils. That’s when the right treatment started.
People who use ipratropium spray often say it’s life-changing. One user wrote: “I used to carry 10 tissues in my pocket. Now I go out without a single one.” Saline rinses get high marks too. “I can smell my coffee again,” said another. “That’s the first time in 10 years.”
But frustration is common. “No one understands,” said a member of a Facebook support group. “My boss thinks I’m being dramatic when I leave the office because the AC is too cold.” And insurance? Many won’t cover ipratropium without prior authorization. It’s a hassle.

What’s Next? The Future of Treatment
Science is catching up. Researchers now know that TRPV1 receptors-those heat-sensing channels-are overactive in nonallergic rhinitis. That’s why heat, spice, and smoke trigger it. A new drug called BCT-100, a TRPV1 blocker, just entered late-stage trials in Europe. Early results show a 55% drop in symptoms. If approved, it could be the first treatment that targets the root cause, not just the symptoms.
Other ideas are in the works: tiny devices that gently zap nasal nerves to reset their signaling, or nasal sprays that block specific nerve pathways. These aren’t available yet, but they’re coming.
For now, the best approach is still simple: identify your triggers, avoid what you can, rinse your nose, and use the right meds. It’s not glamorous, but it works.
How to Get Started Today
Start a symptom diary. Track:
- Temperature and humidity each morning and evening
- What you ate and drank
- Any new products you used (soap, perfume, laundry detergent)
- Medications you took
- When your nose felt worst
Do this for 4-6 weeks. Patterns will emerge. Maybe it’s always after coffee. Or every time the heater turns on. Once you know your triggers, you can start avoiding them.
Try saline rinses twice a day. Buy a neti pot or squeeze bottle from the pharmacy. Use sterile or boiled water. It’s easy to learn, and you’ll feel the difference fast.
If symptoms persist, see an ENT. Ask for a nasal endoscopy and a nasal smear. Don’t settle for “it’s just allergies.” Get the right diagnosis. You deserve better.
Nonallergic rhinitis isn’t dangerous-but it’s exhausting. You shouldn’t have to live with a dripping nose every winter, or avoid your favorite curry, or feel embarrassed when you blow your nose in meetings. It’s treatable. You just need to know how.

Comments
Gran Badshah December 27, 2025 at 16:46
Bro I thought I had allergies till I stopped using my lavender detergent. My nose stopped acting like a faucet. Now I use unscented stuff and rinse with salt water twice a day. Game changer. No more sneezing in meetings.
Ellen-Cathryn Nash December 27, 2025 at 18:00
It’s pathetic how people just accept this as normal. You’re not supposed to be miserable every time you walk outside or eat a burrito. This isn’t ‘just aging’ or ‘being sensitive’-it’s your body screaming for you to stop poisoning yourself with chemicals and then pretending it’s fine. You’re not a victim. You’re complicit.
Samantha Hobbs December 29, 2025 at 12:08
OMG YES. I used to carry 20 tissues in my purse. Then I tried the saline rinse and started avoiding perfume. I didn’t even know I was triggered by my own shampoo. Now I’m basically a new person 😭
Nicole Beasley December 30, 2025 at 13:08
Anyone else get triggered by the AC at work?? Like literally 10 minutes in and I’m crying from the drip. I started wearing a scarf indoors and it’s a miracle. Also, I use a neti pot with distilled water now. No tap water. Ever. 🙏
sonam gupta December 30, 2025 at 23:02
India has this problem too. People think it's dust or cold but its the cheap air fresheners and diesel fumes. No one listens. I use salt water. Done.
Julius Hader December 31, 2025 at 22:39
Man, I wish I’d known this five years ago. I was on Zyrtec for ages. My ENT finally said, ‘You don’t have allergies, you’re just surrounded by irritants.’ I switched to fragrance-free everything and started rinsing. Best decision ever. 😊
Mimi Bos January 1, 2026 at 12:03
so i tried the ipratropium spray and it worked like magic… except i kept getting this weird bitter taste? like, why does my mouth hate me now? but the drip? gone. so worth it. also, i spell ‘neti’ wrong like 80% of the time but i still use it lol
Payton Daily January 3, 2026 at 09:24
You know what this is? It’s the collapse of modern civilization. We’ve filled our homes with chemicals, our air with particulates, our food with spice and steam, and now our bodies are just… overworked. We think we’re civilized. We’re not. We’re walking landfills with noses. The real cure? Move to the mountains. Or go back to nature. Or stop being so damn dependent on everything that’s killing you. I’m not mad. I’m just… disappointed.
Kelsey Youmans January 4, 2026 at 01:54
Thank you for this meticulously researched and compassionate overview. The clinical accuracy paired with practical, patient-centered advice is exceptionally rare in public health communication. I will be sharing this with my colleagues in otolaryngology. The emphasis on nasal smear diagnostics and trigger avoidance over pharmacological band-aids is both scientifically sound and profoundly humane.
Sydney Lee January 4, 2026 at 02:27
Of course the mainstream medical establishment ignores this. They’d rather sell you antihistamines and insurance-denied nasal sprays than admit their diagnostic framework is broken. The fact that TRPV1 blockers are in late-stage trials? That’s the only thing that matters. The rest? Bandwidth. Noise. A system that profits from your ignorance. I’ve been right about this for years. And now, finally, science is catching up. But don’t expect gratitude from the institutions that got it wrong.