Magnesium Hydroxide Dosage Calculator
Determine Your Correct Dose
When you’re stuck in the bathroom for hours, a simple, over‑the‑counter remedy can be a game‑changer. magnesium hydroxide has been used for decades to move the bowels, but many people still wonder how it works, whether it’s safe, and when it’s the right choice.
Magnesium hydroxide is a white, inorganic compound with the formula Mg(OH)₂. It occurs naturally as the mineral brucite and is sold commercially as the liquid “milk of magnesia.” In the body it acts as both an antacid and an osmotic laxative, making it a versatile tool for digestive discomfort.
What Exactly Is Magnesium Hydroxide?
Beyond the chemistry, magnesium hydroxide is essentially a source of magnesium ions and hydroxide ions. When dissolved in water, it creates a mildly alkaline solution that can neutralize stomach acid. This dual action means it can soothe heartburn while also pulling water into the intestines, softening stool and prompting a bowel movement.
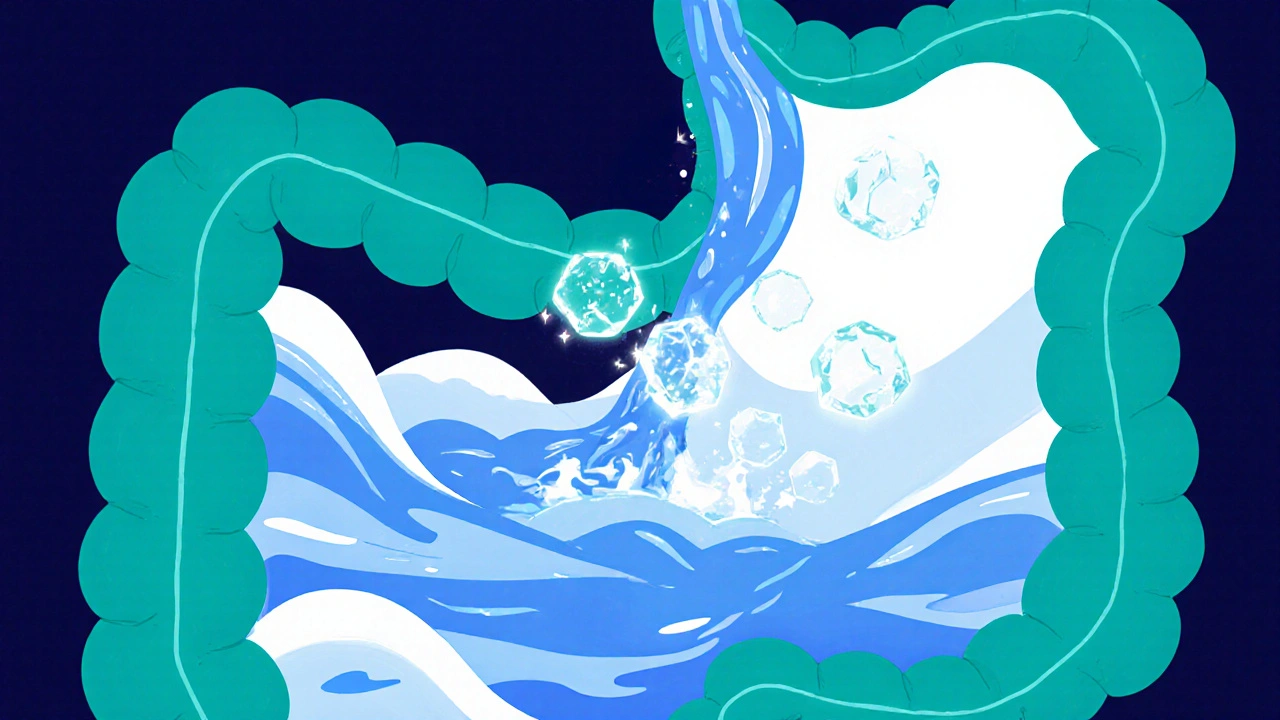
How It Relieves Constipation
Constipation often stems from dehydrated stool that’s difficult to pass. Magnesium hydroxide’s osmotic effect draws water from the bloodstream into the colon, increasing stool volume and triggering peristalsis - the wave‑like muscle contractions that push waste forward. Because the solution is also alkaline, it reduces the irritation that can accompany hard stools, making the passage smoother.
When to Reach for Magnesium Hydroxide
- Occasional constipation: Ideal for short‑term relief when you’ve missed a couple of days without a bowel movement.
- Antacid need: Useful if you’re battling mild heartburn alongside constipation.
- Pregnancy: Generally considered safe in recommended doses, but always check with a healthcare provider first.
Typical adult dose is 30-60 mL (2-4 tablespoons) of the liquid product once daily, or 1-2 grams of the powdered form. Children 2‑12 years old should use 15 mL or 0.5 grams, but pediatric guidance is essential.
Safety Tips and Common Pitfalls
- Stay hydrated: Because magnesium pulls water into the gut, you need to drink plenty of fluids to avoid dehydration.
- Watch electrolytes: Excessive magnesium can upset the balance of potassium and calcium, especially in people with kidney disease.
- Don’t overuse: Regular, daily use may lead to dependence, where the bowels only move with a laxative.
- Avoid interactions: It can interfere with the absorption of certain antibiotics (e.g., tetracyclines) and iron supplements.
Magnesium Hydroxide vs. Other Common Laxatives
| Product | Type | Mechanism | Onset (hours) | Typical Adult Dose | Pros | Cons |
|---|---|---|---|---|---|---|
| Magnesium hydroxide | Osmotic/Antacid | Draws water into colon, neutralizes acid | 4‑6 | 30‑60 mL liquid or 1‑2 g powder | Gentle, also eases heartburn | May cause loose stools, electrolyte shift |
| Psyllium husk | Bulk‑forming | Adds fiber, absorbs water | 12‑24 | 5‑10 g mixed with water | Improves overall gut health | Needs plenty of fluid, may cause bloating |
| Bisacodyl | Stimulant | Stimulates intestinal muscles | 6‑12 | 5‑10 mg oral tablet | Fast‑acting for stubborn cases | Can cause cramping, dependency risk |
| Lactulose | Osmotic | Fermentation produces acids, draws water | 12‑48 | 15‑30 mL syrup | Gentle, used for chronic constipation | May cause gas, taste issues |
| Docusate sodium | Stool softener | Reduces surface tension of stool | 12‑24 | 100‑200 mg capsule | Easy on the gut | Less effective for severe blockage |
Maximizing the Effectiveness of Magnesium Hydroxide
- Take with a full glass of water: This ensures enough fluid is available for the osmotic action.
- Combine with fiber‑rich foods: Whole grains, fruits, and vegetables add bulk, helping the magnesium work more efficiently.
- Choose the right timing: Evening doses often lead to a next‑morning bathroom visit, fitting most schedules.
- Avoid high‑dose antacids simultaneously: They can reduce the laxative effect.
- Monitor for side effects: If you notice persistent diarrhea, abdominal pain, or muscle weakness, stop use and consult a professional.

When Magnesium Hydroxide Isn’t the Best Choice
If you have any of the following conditions, consider alternatives:
- Severe kidney disease - reduced ability to clear excess magnesium.
- Intestinal blockage - osmotic laxatives can worsen obstruction.
- Electrolyte disorders - especially low potassium or calcium.
In these cases, a doctor might suggest a fiber supplement or a different class of laxative that doesn’t rely on magnesium.
Quick Checklist Before You Use Magnesium Hydroxide
- Confirm you’re not pregnant without medical advice.
- Check current medications for potential interactions.
- Ensure you’ll drink at least 8 cups of water daily.
- Start with the lowest effective dose.
- Set a reminder to monitor bowel movements for the next 24‑48 hours.
Frequently Asked Questions
Can I use magnesium hydroxide every day?
Occasional use is safe, but daily reliance can lead to electrolyte imbalance and reduced natural bowel function. Consult a healthcare provider for long‑term plans.
Is magnesium hydroxide safe for children?
Children can use a reduced dose (about 15 mL for ages 2‑12), but you should always follow pediatric guidance and avoid giving it to infants without doctor approval.
How quickly will I feel relief?
Most adults notice a bowel movement within 4‑6 hours after a single dose. If you don’t see results after 12 hours, consider a higher dose or an alternative laxative.
Can magnesium hydroxide interact with other meds?
Yes. It can reduce absorption of tetracycline antibiotics, iron supplements, and some bisphosphonates. Take those meds at least 2 hours before or after magnesium hydroxide.
What should I do if I get diarrhea?
Stop the magnesium hydroxide immediately, increase fluid intake, and consider an electrolyte solution. If diarrheal symptoms persist beyond 24 hours, seek medical advice.
Magnesium hydroxide remains a trusted, affordable option for occasional constipation, especially when paired with proper hydration and a balanced diet. By understanding its action, dosing, and limits, you can safely reap its benefits without unnecessary side effects.

Comments
Penny Reeves October 19, 2025 at 12:43
Magnesium hydroxide, chemically Mg(OH)₂, is not merely a kitchen staple but a paradigmatic example of a weak base that buffers gastric acidity while simultaneously exerts an osmotic gradient in the colon. The dual functionality stems from its dissociation into Mg²⁺ and OH⁻ ions, which neutralize HCl in the stomach and draw water into the intestinal lumen. This mechanistic nuance is often glossed over in lay summaries that treat it as "simple laxative." In reality, the pharmacodynamics involve a delicate balance between pH modulation and electrolyte movement, which explains the occasional side‑effects of loose stools and altered potassium levels. Thus, when you reach for "milk of magnesia," you are invoking a chemically sophisticated process that belies its over‑the‑counter façade.
Nicole Boyle October 19, 2025 at 12:53
From a gastroenterological perspective, the osmotic activity of magnesium hydroxide is mediated by its ability to increase the luminal osmolarity, thereby promoting water influx via paracellular pathways. I’ve observed that coupling the agent with a diet rich in soluble fiber-like pectin or β‑glucan-optimizes stool bulk without compromising the alkaline buffer capacity. Keep in mind the Henderson–Hasselbalch equation when evaluating its antacid efficacy; the pKa of the hydroxide moiety dictates the degree of acid neutralization. Hydration status remains the primary variable; a minimum of 2 L of fluid per day is advisable to prevent iatrogenic dehydration.
dennis turcios October 19, 2025 at 13:03
While the article extols magnesium hydroxide as a universally safe option, it conveniently omits the fact that chronic use can precipitate a hypomagnesemic state, especially in patients with subclinical renal insufficiency. The oversimplified dosing chart neglects weight‑based adjustments, which are critical for achieving therapeutic efficacy without overshooting the therapeutic window. Moreover, the interaction profile with tetracyclines is not a peripheral concern; concomitant administration can reduce antibiotic bioavailability by upwards of 40 %. If you’re looking for a one‑size‑fits‑all remedy, you’re better off consulting a qualified practitioner rather than trusting a generic OTC label.
Felix Chan October 19, 2025 at 13:13
Hey folks, if you’re stuck on the throne, a glass of milk of magnesia before bedtime can work like a charm and have you up and about in the morning. Just remember to pair it with a tall glass of water and maybe a banana for some extra potassium. Stay positive and your gut will thank you!
Thokchom Imosana October 19, 2025 at 13:23
The widespread promotion of magnesium hydroxide as a benign, over‑the‑counter laxative is, in my view, a textbook case of corporate pharmaco‑politics masquerading as public health guidance. What most consumers fail to see is that the active ingredient, Mg(OH)₂, is exfiltrated from mining operations heavily subsidized by multinational conglomerates that control vast swathes of the global mineral supply chain. By commodifying a naturally occurring mineral such as brucite, these entities effectively lock the market into a cycle of dependency where the layperson is encouraged to self‑medicate rather than seek professional evaluation. The subtle shift in pH that magnesium hydroxide induces is not merely a benign neutralization; it alters the intestinal microbiome in ways that are still being uncovered by a handful of independent researchers barred from mainstream journals. Moreover, the osmotic draw of water into the colon can perturb electrolyte homeostasis, a fact that is conveniently buried beneath the “safe for occasional use” disclaimer printed on the label. Critics who highlight the risk of hypermagnesemia are often dismissed as alarmist, yet a meta‑analysis published in an obscure open‑access repository demonstrated a statistically significant rise in serum magnesium among chronic users. This data, however, is rarely amplified by the mainstream media, which receives generous advertising revenues from the very manufacturers whose products are under scrutiny. Adding to the concern, the antacid component can interfere with the absorption of essential nutrients such as calcium and iron, potentially contributing to long‑term skeletal demineralization. The correlation between prolonged magnesium hydroxide intake and reduced bone mineral density has been hinted at in a small cohort study from a university that was forced to retract its findings under pressure from industry sponsors. One cannot ignore the regulatory loophole that classifies magnesium hydroxide as a “dietary supplement” rather than a pharmaceutical agent, thereby evading the rigorous safety testing required for prescription drugs. This loophole enables manufacturers to adjust concentrations arbitrarily, sometimes resulting in formulations that are more potent than the FDA‑approved standard, all without a single warning label amendment. Consumers, lulled into a false sense of security by the product’s gentle branding-“milk of magnesia”-are thereby exposed to a hidden pharmacological risk that is systematically downplayed. The pattern mirrors historical episodes where benign‑looking compounds were later revealed to carry systemic toxicity once large‑scale epidemiological data emerged. In the context of pregnancy, the recommendation to use magnesium hydroxide “generally considered safe” is particularly disquieting, given the paucity of robust teratogenic studies. It is incumbent upon informed individuals to scrutinize the provenance of such OTC remedies and to demand transparent, peer‑reviewed evidence before integrating them into daily health regimens. Until the veil of corporate benevolence is lifted, we should approach magnesium hydroxide with the same caution we afford any pharmacologically active compound, recognizing that “natural” does not inherently equate to “harmless.”
Bobby Marie October 19, 2025 at 13:33
Don’t forget to check the expiration date before you pour it down.
Christopher Burczyk October 19, 2025 at 13:43
From a pharmacokinetic standpoint, the absorption of magnesium ions following oral administration of magnesium hydroxide is negligible, as the compound primarily exerts its laxative effect within the gastrointestinal lumen. The resultant increase in intraluminal osmolarity facilitates a passive water influx, thereby softening fecal matter and stimulating colonic peristalsis. It is imperative to emphasize that systemic bioavailability remains low, which mitigates the risk of significant serum magnesium elevation in healthy individuals. Nonetheless, in patients with compromised renal excretory function, even modest accumulations can precipitate hypermagnesemia, warranting dose adjustments or alternative therapies. Consequently, clinicians should assess renal function and concomitant medication profiles prior to recommending routine magnesium hydroxide use.
Caroline Keller October 19, 2025 at 13:53
It’s infuriating how people treat their bodies like disposable junkyards, flushing away natural balance for a quick fix and then blame the very remedy they abused. The moral of the story is simple: respect your gut or it will betray you in the most embarrassing ways. No amount of "milk" can mask the shame of neglecting proper hydration and dietary fiber. Stop looking for shortcuts and start listening to your body, because the consequences are far too real to ignore.
ashanti barrett October 19, 2025 at 14:03
I understand the frustration of dealing with occasional constipation, and I want to point out that building a routine that includes regular physical activity can dramatically improve bowel regularity. Incorporating a balanced intake of soluble and insoluble fiber, alongside adequate water consumption, creates a synergistic environment that reduces reliance on pharmacological agents. When magnesium hydroxide is used, it should be positioned as an occasional adjunct rather than a primary solution. Monitoring stool consistency and frequency for trends will empower you to make informed adjustments without fear of dependence. This proactive approach respects both your immediate comfort and long‑term gastrointestinal health.