What Is a Drug Formulary and Why It Matters for Seniors
A drug formulary is simply a list of medications your insurance plan covers. It’s not just a catalog-it’s a pricing system. Each drug is placed in a tier, and that tier determines how much you pay out of pocket when you fill a prescription. For seniors on Medicare Part D or private plans, this can mean the difference between paying $5 or $150 for the same pill.
Formularies are updated every year, usually on January 1st. But they can also change mid-year. If your blood pressure med suddenly jumps from Tier 1 to Tier 4, your monthly cost could spike overnight. That’s not a mistake-it’s standard practice. And if you don’t check, you won’t know until you’re at the pharmacy counter.
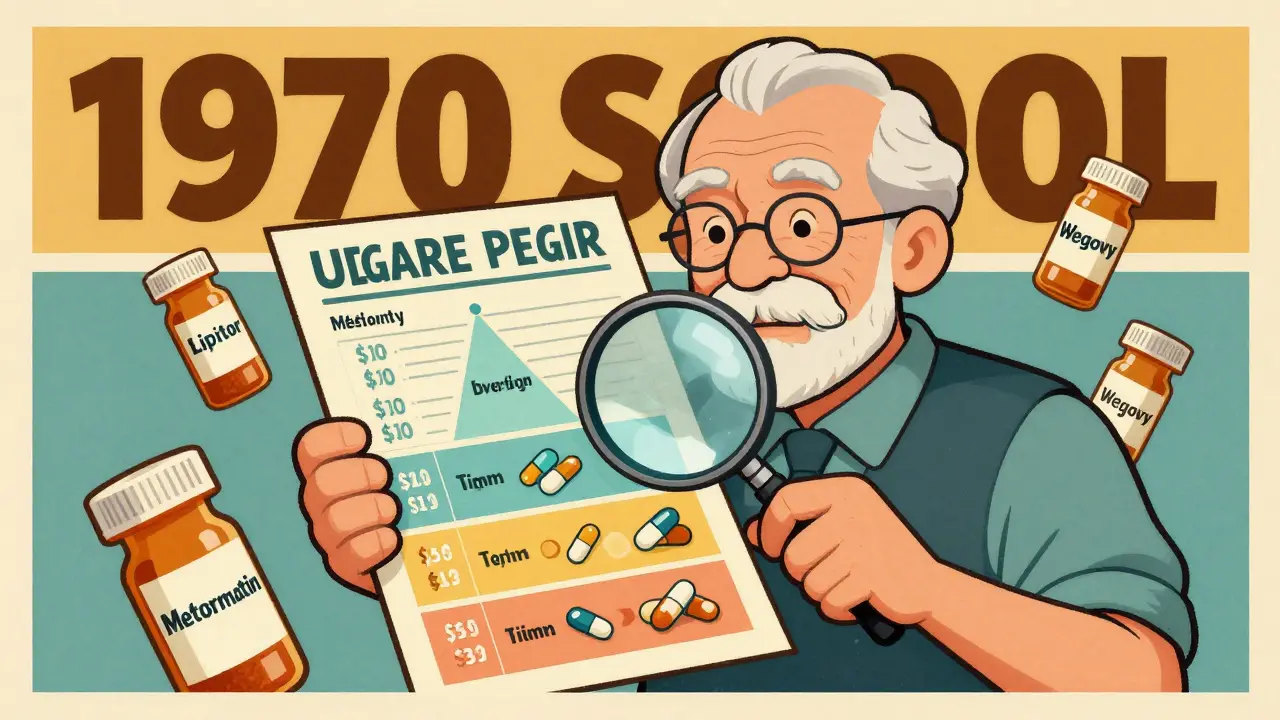
How Tier Systems Work: 3-Tier, 4-Tier, 5-Tier Explained Simply
Most plans use one of three tier structures. Here’s what they look like in real dollars:
- 3-Tier: Tier 1 = generics (usually $5-$10), Tier 2 = brand-name drugs ($30-$50), Tier 3 = specialty drugs ($100+)
- 4-Tier: Tier 1 = preferred generics ($0-$10), Tier 2 = non-preferred generics and some brands ($15-$40), Tier 3 = high-cost brands ($50-$80), Tier 4 = specialty drugs ($100-$300)
- 5-Tier: Adds more granularity: Tier 1 = preferred generics, Tier 2 = non-preferred generics, Tier 3 = preferred brands, Tier 4 = non-preferred brands, Tier 5 = specialty drugs (like GLP-1 weight loss meds)
Don’t assume your plan’s tiers match another’s. A drug like metformin might be Tier 1 with one insurer and Tier 2 with another. That’s why checking your specific plan is non-negotiable.
Where to Find Your Plan’s Formulary-Step by Step
Every Medicare Part D or private insurance plan has an online formulary tool. Here’s how to use it:
- Go to your insurer’s website (Cigna, Humana, Excellus BCBS, UnitedHealthcare, etc.)
- Look for “Drug List,” “Formulary,” or “Find a Drug” in the member portal
- Enter your medication’s name exactly as it appears on the prescription (brand or generic)
- Check the tier, copay amount, and any restrictions like prior authorization or step therapy
Some plans, like Cigna and Simply Prescriptions, let you search by drug name, condition, or even compare alternatives. If you can’t find the tool, call customer service. They’re required by law to help you.
How to Spot Mid-Year Formulary Changes
Plans can change your drug’s tier at any time. But they must tell you-if you’re taking that drug. Look for:
- A letter in the mail from your insurer (sent at least 60 days before the change, unless it’s a safety issue)
- An email or secure message in your online account
- A notice when you try to refill your prescription at the pharmacy
Don’t wait for the letter. Check your formulary every October, before Open Enrollment. That’s when plans release their next year’s list. If your medication moved up a tier, you’ll have time to switch plans or ask for an exception.
What to Do When Your Drug Gets Moved to a Higher Tier
If your drug suddenly costs more, you have options:
- Ask your doctor for a generic or alternative. Many brand-name drugs have cheaper generics that work just as well. For example, if your brand-name statin moved to Tier 4, ask if atorvastatin (generic Lipitor) is covered on Tier 1.
- Request a formulary exception. You can ask your plan to cover your drug at a lower tier if it’s medically necessary. Your doctor fills out a short form. Approval rates range from 55% to 82%, depending on your plan and evidence of need.
- Use a 30-day transition supply. If your drug was removed or moved up, most plans must give you at least 30 days of your current prescription while you switch or appeal.
Many seniors don’t know they can request exceptions. In fact, 31% of users in a GoodRx survey said they didn’t understand how to ask. Don’t be one of them. Call your plan or talk to your pharmacist.
Common Pitfalls and How to Avoid Them
Here are the top mistakes seniors make with formularies:
- Assuming your plan didn’t change. Even if you stayed with the same insurer, the formulary might’ve been rewritten. Always recheck.
- Only checking during Open Enrollment. Mid-year changes happen. Check your formulary every 6 months if you’re on multiple meds.
- Not using your pharmacist. Pharmacists see formulary updates daily. Ask them: “Is my med still covered at the same price?”
- Ignoring specialty drug tiers. New weight loss drugs like Wegovy and Ozempic are being moved into Tier 5. If you’re on one, expect costs to rise.
Pro tip: Keep a printed copy of your current formulary. Highlight your meds. Update it every time you get a notice. It’s easier than scrolling through a website when you’re stressed.
Free Resources That Actually Help
You don’t have to figure this out alone. Here are real, free tools:
- Medicare.gov’s Plan Finder - Compare all Part D plans side by side. Enter your drugs and see which plan has the lowest total cost.
- SHIP (State Health Insurance Assistance Program) - Free, local counselors who walk you through formularies. Call 1-877-839-2675 or visit medicare.gov/ship.
- GoodRx - Not insurance, but shows cash prices. Sometimes paying cash is cheaper than your copay, especially for Tier 4 drugs.
- Pharmacist consultations - Many pharmacies offer free med reviews. Ask for one if you take 5+ drugs.
What’s Changing in 2026 and Beyond
Formularies are getting more complex. By 2026, over half of top-selling drugs will be specialty medications-meaning higher tiers and more restrictions. GLP-1 drugs for weight loss are already being pushed into Tier 5, even if they’re used for diabetes. That’s driving up costs for seniors who rely on them.
CMS is testing a simplified 4-tier model for 2025 to reduce confusion. But until then, the burden is on you to stay informed. Plans are required to clearly state change dates and your right to appeal. Use that information.
Final Checklist: Your Formulary Action Plan
Do this every October and every six months after:
- ✅ List all your current prescriptions (brand and generic)
- ✅ Go to your insurer’s formulary tool and check each one
- ✅ Note the tier and copay for each
- ✅ Compare with last year’s list-did anything move up?
- ✅ Call your pharmacist or SHIP counselor if unsure
- ✅ Ask your doctor: “Is there a cheaper, equally effective option?”
- ✅ Save a copy of your formulary and update it when you get a notice
Formularies aren’t designed to be easy. But they’re not meant to trap you either. With a little effort, you can avoid surprise bills and keep your meds affordable.
Comments
Shanahan Crowell January 4, 2026 at 09:44
This is GOLD. Seriously, I printed this out and taped it to my fridge. My grandma didn’t know her insulin went from $12 to $147 until she got hit at the counter. Now she checks every October like clockwork. Thank you for making this so damn clear!
Kerry Howarth January 6, 2026 at 08:40
Check your formulary every six months. Always.
Joy F January 7, 2026 at 08:36
Let’s be real-this isn’t just about formularies. It’s about the quiet erosion of dignity in American healthcare. They turn your life into a spreadsheet, then charge you extra to read it. GLP-1 drugs? They’re not ‘specialty,’ they’re life-saving. But hey, let’s tier them like luxury handbags. 🤡
Haley Parizo January 8, 2026 at 16:05
This system is a weapon. It’s not broken-it’s designed to break people. You think seniors are supposed to become pharmacologists just to afford their meds? No. We’re supposed to die quietly so the shareholders get their dividend. The fact that you’re even asking how to navigate this? That’s resistance.
Ian Detrick January 10, 2026 at 12:33
I’ve been helping my dad with his meds for years. The hardest part isn’t finding the formulary-it’s convincing him to check it. He thinks if it worked last year, it’ll work this year. But the system doesn’t care about habit. It only cares about profit margins. That’s why I print the list, highlight everything, and put it in his wallet. No excuses.
Brittany Wallace January 11, 2026 at 06:09
This is the kind of post that makes me believe in Reddit again 😊 I’m sending this to my mom’s group chat. She’s on 7 meds and thinks her pharmacy is ‘just being difficult.’ Nope. It’s the formulary. Time to arm her with knowledge. Thank you!
Palesa Makuru January 12, 2026 at 12:52
I’m from South Africa and honestly? This is wild. We have our own mess, but at least our public system doesn’t tier drugs like they’re designer sneakers. You people pay $300 for a pill? And you’re supposed to be grateful? I don’t understand your system. It’s not healthcare. It’s a casino with pills.
Lori Jackson January 12, 2026 at 18:05
If you’re not using GoodRx, you’re literally leaving money on the table. I had a friend who paid $120 for a Tier 4 drug-until she checked GoodRx and found the cash price was $28. She cried. Not from joy-from rage. Why does this even exist? Why are we this stupid?
veronica guillen giles January 14, 2026 at 07:26
Oh sweetie, you think you’re the first person to write this? The pharmacist at CVS told me this exact thing in 2018. But sure, let’s act like this is new news. Meanwhile, my neighbor’s husband died because he skipped his meds after the tier jump. And now we’re all just… commenting? Cute.
Ian Ring January 14, 2026 at 19:48
I’ve shared this with my sister-in-law in Ohio-she’s on Medicare Advantage and had no idea about mid-year changes. She’s now checking every month. Thank you for the clarity. And yes, I printed it. With a highlighter. And a coffee stain. 🤷♂️☕
erica yabut January 15, 2026 at 23:14
Let me guess-this post was sponsored by Humana. 'Oh look, here’s how to navigate the trap!' No. The real solution is single-payer. The real solution is not letting corporations decide if your life is worth $5 or $150. But sure, let’s keep pretending we’re solving this by checking websites. I’m exhausted.
Vincent Sunio January 17, 2026 at 11:10
The assertion that 'many brand-name drugs have cheaper generics that work just as well' is statistically misleading. Bioequivalence does not equal clinical equivalence. For patients with complex comorbidities, switching to a generic may result in increased hospitalizations. This post oversimplifies a deeply complex pharmacoeconomic issue.
JUNE OHM January 19, 2026 at 10:10
This is all part of the Great Pharma Cover-Up. They’re using tier systems to slowly kill off seniors so they can push the new AI-driven 'health optimization' programs. You think they care if you live? They just want your data. And your Social Security. Wake up. 🚨💉
Tiffany Channell January 20, 2026 at 02:58
I’ve seen this happen too many times. One woman I know was on metformin for 12 years. January 1st, it moved to Tier 4. She stopped taking it. Got hospitalized. The plan didn’t cover her ER visit because she was 'non-compliant.' They didn’t tell her. She didn’t know. This isn’t negligence. It’s predation.
Liam Tanner January 20, 2026 at 14:25
If you’re reading this and you’re not helping someone older navigate this? Do it. Just sit with them. Open the website. Type in the drug. Show them the tier. Make them feel safe. This isn’t just about money. It’s about not feeling powerless. You can be the person who changes that.