Most people don’t realize that the pill they’re paying $200 for might be almost identical to one that costs $4. Generic drugs aren’t second-rate-they’re the same medicine, just without the brand name. The FDA requires them to have the exact same active ingredient, strength, dosage, and effect as the brand-name version. But if you’ve never brought it up with your doctor, you might be overpaying without even knowing it.
Why Generics Are Just as Good
Let’s clear up the biggest myth: generics aren’t weaker. They’re required by law to deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug. The FDA calls this bioequivalence, and it means your body processes the generic exactly like the brand. For 95% of medications, there’s no difference in how well they work or how you feel taking them.
Think of it like buying a plain white T-shirt versus a designer one. Same cotton, same fit, same comfort. The only difference is the label. The same goes for generic lisinopril, sertraline, or metformin. In fact, 89% of all prescriptions filled in Medicare Part D are for generics, because doctors and pharmacists know they work.
Even when multiple companies make the same generic, the FDA checks each batch. If one version doesn’t meet the standard, it’s pulled. And when competition kicks in-usually within a year or two after the brand patent expires-prices can drop 50% to 95%. A drug that costs $300 a month might drop to $15. That’s not a rumor. That’s data from the FDA and Medicare reports.
When Generics Might Not Be the Best Choice
There are exceptions. About 5% of medications fall into a category called narrow therapeutic index (NTI) drugs. These are medicines where even tiny changes in blood levels can cause big problems. Think blood thinners like warfarin, thyroid meds like levothyroxine, or seizure drugs like phenytoin.
For these, your doctor might prefer you stick with one brand or one generic manufacturer. Why? Because switching between different generics-even if they’re all FDA-approved-can sometimes cause small shifts in how your body responds. One study from Johns Hopkins documented a patient whose thyroid levels went off after switching generic brands. That’s not common, but it’s real.
That’s why you need to ask: “Is this one of those drugs where consistency matters?” If the answer is yes, then sticking with one version-even if it’s the brand-is a valid choice. But if it’s not an NTI drug, there’s no medical reason to pay more.
How to Bring It Up Without Sounding Like You’re Trying to Cut Corners
Doctors aren’t always aware of which generics are available or covered by your insurance. Many don’t track the latest price drops or new generic approvals. That’s why you need to lead the conversation-not in a demanding way, but as a partner in your care.
Instead of saying, “Can I get the generic?” try: “I’m looking for the most effective option at the best price. Is there a generic version of this medication that would work for me?”
This shifts the focus from cost to safety and effectiveness. It tells your doctor you care about doing the right thing, not just saving money. And it opens the door for them to explain if there’s a reason to avoid it.
Bring a simple list to your appointment. Write down the name of the drug, the dose, and what you’re paying now. If you can, check your pharmacy’s cash price for the generic. For example: Nexium (brand) costs $284 for 30 pills. Omeprazole (generic) costs $4. That’s not a typo. That’s real.
Timing Matters: Ask Before You Get the Prescription
Don’t wait until you’re at the pharmacy counter. That’s when you’re stuck with a bill you didn’t expect. Ask during your appointment. If your doctor says, “I’ll write the prescription,” follow up with: “Can you write it so the pharmacist can substitute a generic if available?”
Most states let pharmacists switch to generics automatically unless the doctor says “Do Not Substitute.” But if your doctor doesn’t mention it, they might not realize the generic exists. Or they might assume you already know.
And if your doctor says, “No, you need the brand,” ask why. Specifically: “Is this because it’s a narrow therapeutic index drug, or is there another reason?” If they can’t give you a clear, evidence-based answer, it’s worth getting a second opinion or asking your pharmacist to check.
What Your Pharmacist Can Do for You
Pharmacists are your hidden allies. They see every prescription, know which generics are in stock, and understand insurance coverage better than most doctors. If you get to the pharmacy and the pharmacist says, “We can give you the generic,” but your doctor didn’t specify it, you’re still good to go-unless the script says “Do Not Substitute.”
And if your doctor didn’t mention generics at all, ask your pharmacist: “Is there a generic version of this drug that’s covered by my plan?” Many pharmacists will call your doctor’s office to suggest a switch if it’s safe and cheaper. They do this all the time.
Insurance and Costs: The Real Numbers
Your insurance plan makes a huge difference. Medicare Part D fills 89% of prescriptions with generics. Commercial plans? Around 72%. That means if you’re on a private plan, you might have more room to save.
Check your plan’s formulary. Most have a tier system. Generics are usually Tier 1-lowest cost. Brands are Tier 3 or 4. You could be paying $50 more just because your script says “brand only.”
And here’s a pro tip: sometimes the cash price for a generic is lower than your insurance copay. Always ask the pharmacist: “What’s the cash price for the generic?” You might pay less without using insurance at all.
For example, a patient with rheumatoid arthritis switched from Humira (brand) to adalimumab (generic) and saved $1,820 a month. That’s not an outlier. That’s the norm for biologics now that generics are entering the market.
What to Do If Your Doctor Says No
If your doctor refuses to switch you to a generic, don’t just accept it. Ask for the reason. Is it because of NTI? Is it because of your specific condition? Is it because they’ve seen better results with the brand in your case?
If they say, “I just prefer the brand,” that’s not a medical reason. You can say: “I understand you’re used to prescribing this, but I’d like to explore whether the generic would work just as well for me. Can we try it and check in after a few weeks?”
Most doctors will agree to a trial. If they don’t, you can ask for a referral to a pharmacist or a specialist who works with cost-effective prescribing. Many hospitals now have medication therapy management programs that help patients switch to generics safely.
Real People, Real Savings
AARP surveyed 12,500 seniors in 2022. Of those who asked their doctor about generics, 68% successfully switched. They saved an average of $427 a year. One woman switched from brand-name Zoloft to sertraline and saved $360 a year. She said she didn’t notice any difference in her mood-just a lighter wallet.
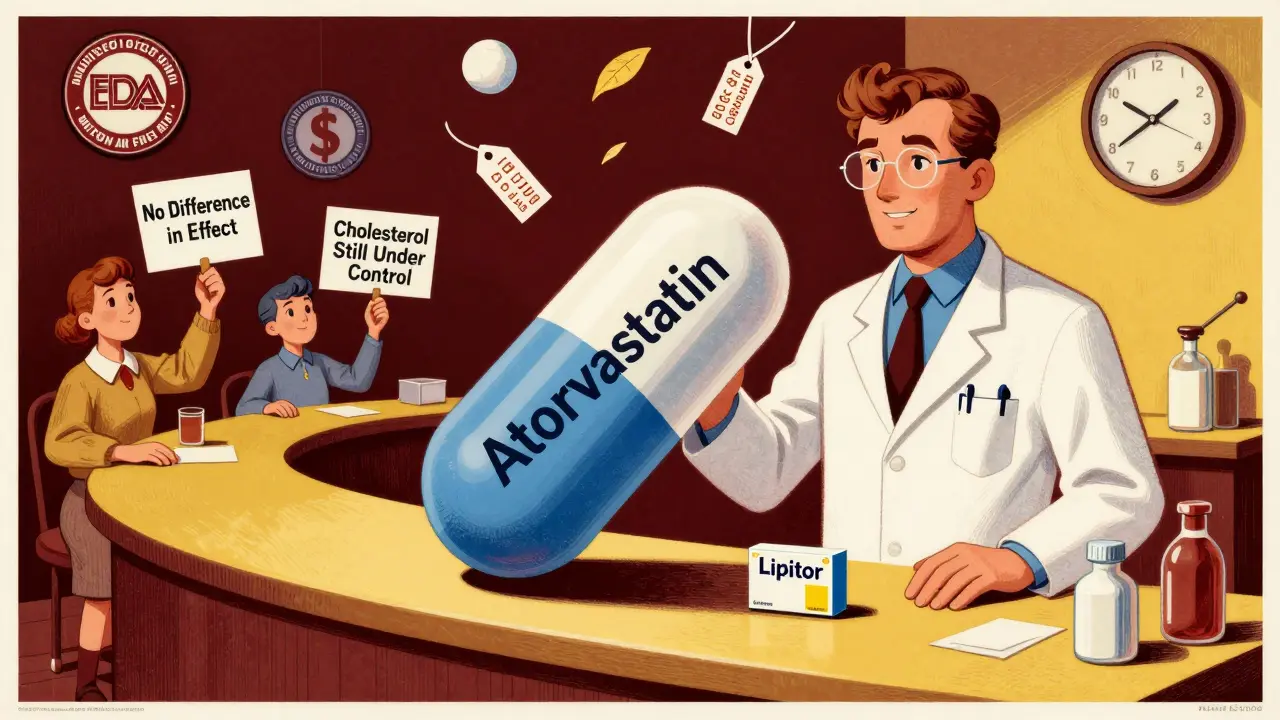
Another man switched from brand-name Lipitor to atorvastatin. His cholesterol stayed under control. His out-of-pocket cost dropped from $80 to $5 a month.
These aren’t rare stories. They’re everyday wins. And they happen because people asked.
Next Steps: What to Do Today
- Look at your last prescription. Is it a brand name? Check Drugs.com or GoodRx for the generic name and price.
- Write down your top 3 medications. For each, ask: Is there a generic? Is it NTI?
- Next time you see your doctor, say: “I’d like to make sure I’m on the most cost-effective version of these meds that still works well.”
- If you’re on a long-term medication, ask your pharmacist to review your list for savings opportunities.
- Don’t be afraid to ask twice. If you get a “no” the first time, come back with data. Bring a printout of the generic price. Show them the FDA’s stance on bioequivalence.
You’re not asking for a discount. You’re asking for the same medicine at the same price. And you deserve it.
Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of medications. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. Studies show that 78% of patients who switched to generics reported no difference in effectiveness. Generics are tested to ensure they deliver the same amount of medicine into your bloodstream at the same rate. The only differences are in color, shape, or inactive ingredients-which don’t affect how the drug works.
Why do some doctors hesitate to prescribe generics?
Some doctors aren’t up to date on which generics are available or covered by insurance. Others may have seen rare cases where switching caused issues-usually with narrow therapeutic index drugs like warfarin or levothyroxine. But for 95% of medications, there’s no medical reason to avoid generics. Many doctors also assume patients want the brand because of marketing, not because it’s better.
Can I switch from a brand to a generic mid-treatment?
Yes, for most medications. If you’re on a drug like high blood pressure or cholesterol medicine, switching is safe and common. For narrow therapeutic index drugs, your doctor may recommend staying on the same manufacturer to avoid small changes in blood levels. Always talk to your doctor or pharmacist before switching, especially if you’re on multiple meds or have a chronic condition.
What if my insurance won’t cover the generic?
That’s rare, but it can happen. First, check if the generic is on your plan’s formulary. If it’s not, ask your pharmacist to request a formulary exception. Sometimes, the generic is cheaper than your copay-so pay cash instead. You can also ask your doctor to write a letter of medical necessity if there’s a specific reason you need the brand. But for most drugs, the generic is covered and preferred.
How do I know if my medication has a generic version?
Look up your drug on the FDA’s Orange Book or use a free site like GoodRx or Drugs.com. Type in the brand name, and it will show if a generic is available. If the drug was approved after 2010, it might still be under patent. But most common meds-like metformin, lisinopril, or simvastatin-have had generics for years. If you’re unsure, ask your pharmacist. They can tell you instantly.

Comments
Erica Vest December 18, 2025 at 13:53
Generic drugs are held to the exact same FDA standards as brand-name medications. The bioequivalence requirement means the active ingredient must hit your bloodstream at the same rate and extent. There’s no clinical evidence supporting superior outcomes with branded drugs for 95% of prescriptions. This isn’t marketing-it’s pharmacology.
Chris Davidson December 20, 2025 at 00:13
People pay extra for the brand because they think it works better but it's the same damn pill just without the fancy logo
Kinnaird Lynsey December 21, 2025 at 18:14
I used to be skeptical too until I switched from brand-name Prilosec to omeprazole and saved $200/month. No change in my acid reflux. No weird side effects. Just… cheaper. Funny how we’ve been conditioned to equate price with quality when it’s just packaging.
Mike Rengifo December 22, 2025 at 16:54
My pharmacist once called my doctor to switch me from brand to generic for my blood pressure med. Doctor was surprised it even existed. Turned out the generic was $5. I paid $80 before. That’s not saving money. That’s getting robbed.
Moses Odumbe December 24, 2025 at 07:25
GENERIC = SAME DRUG 💯
BRAND = SAME DRUG + $200 TAX 🤡
Stop paying for the logo. The FDA doesn’t care what color the pill is. Your body doesn’t care either. Just ask your doc. Or better yet-ask your pharmacist. They know way more than you think.
Meenakshi Jaiswal December 25, 2025 at 12:25
As a pharmacist in India, I see this every day. Generic metformin costs less than a cup of chai. Patients often assume the expensive one is better. But when we explain bioequivalence, their eyes light up. It’s not about cutting corners-it’s about access. Everyone deserves effective medicine without financial stress.
Tim Goodfellow December 26, 2025 at 08:34
Imagine if you bought a car and paid double because it had a fancy emblem on the hood. That’s what we do with pills. The engine-the active ingredient-is identical. The paint job? Cosmetic. The FDA’s the mechanic who makes sure both versions run the same. Stop overpaying for branding. It’s not luxury-it’s a scam dressed in white lab coats.
mark shortus December 27, 2025 at 21:20
THIS IS A CONSPIRACY. BIG PHARMA KNOWS YOU’RE STUPID ENOUGH TO PAY $300 FOR A PILLS THAT COSTS $4. THEY PUSH BRAND NAMES LIKE A RELIGION. DOCTORS? THEY’RE PAID TO KEEP YOU DEPENDENT. I SWITCHED TO GENERIC ZOLOFT AND MY MIND DIDN’T MELT. I DIDN’T DIE. I SAVED $4,000 A YEAR. THEY’RE AFRAID OF YOU FINDING OUT.
Elaine Douglass December 28, 2025 at 08:43
I didn't know generics were the same until my mom told me about her blood pressure med. She switched and said she felt the same. I'm gonna ask my doctor next time.
Takeysha Turnquest December 30, 2025 at 01:05
We’ve been taught that value is measured in price tags. But medicine isn’t a luxury good. It’s a biological necessity. The fact that we accept paying 10x for the same molecule is a reflection of a system that commodifies healing. The pill doesn’t care if it’s labeled A or B. Only the bank account does.
Vicki Belcher December 30, 2025 at 15:18
YAYYYYY! 💖 So glad someone finally said this! I switched my cholesterol med to generic and cried happy tears at the pharmacy. $80 → $5. My doctor was shocked I even knew to ask. You’re not being cheap-you’re being SMART. Keep speaking up!! 🙌
Aboobakar Muhammedali December 31, 2025 at 15:15
My cousin in Delhi takes the same generic atorvastatin as my cousin in Texas. Same pill. Same results. Same price in local currency. The system tries to make us think medicine is different by country-but science doesn’t have borders. The FDA, WHO, and India’s CDSCO all agree: generics work. We just need to stop being scared of the word ‘generic’.
Laura Hamill January 1, 2026 at 04:59
THEY WANT YOU TO THINK GENERICS ARE DANGEROUS. THEY’RE LYING. THE GOVERNMENT AND PHARMA ARE IN BED TOGETHER. YOU THINK YOUR DOCTOR CARES? THEY GET BONUS FOR PRESCRIBING BRANDS. I SAW A REPORT ON A SECRET WEBSITE. THEY USE INACTIVE INGREDIENTS TO MAKE YOU SICK ON PURPOSE. I SWITCHED TO GENERIC AND MY HEADACHE GOT WORSE. IT’S A TRAP.