Osteoporosis Drug Decision Aid
Do you have a history of blood clots or deep vein thrombosis (DVT)?
Key Takeaways
- Evista (raloxifene) is an oral SERM that lowers spine‑fracture risk but does not prevent hip fractures.
- Bisphosphonates (e.g., alendronate, zoledronic acid) are the most widely used first‑line drugs for both spine and hip.
- Denosumab, given as a subcutaneous injection every six months, works for patients who cannot tolerate oral meds.
- Hormone replacement therapy (HRT) can protect bone but carries higher breast‑cancer and cardiovascular risks.
- Choosing the right drug depends on fracture risk, kidney function, tolerance of side‑effects, dosing convenience, and cost.
Osteoporosis silently weakens bone, especially after menopause. When a doctor prescribes a medication, the biggest question is: which one fits my health profile best? This guide breaks down Evista (raloxifene) and the most common alternatives, so you can see the pros, cons, and ideal patient scenarios at a glance.
What is Evista (Raloxifene)?
Evista is a selective estrogen receptor modulator (SERM) approved for the prevention and treatment of post‑menopausal osteoporosis. It mimics estrogen in bone, slowing the breakdown of bone tissue, while acting as an estrogen blocker in breast and uterus.
- Mechanism: Binds estrogen receptors on bone cells, reducing osteoclast activity.
- Efficacy: Reduces vertebral (spine) fracture risk by about 30‑40% in clinical trials; does not significantly lower hip‑fracture rates.
- Dosing: 60mg tablet taken once daily with or without food.
- Key side‑effects: Hot flashes, leg cramps, and a small increase in deep‑vein thrombosis (DVT) risk.
- Contra‑indications: History of blood clots, active liver disease, or pregnancy.
Common Alternatives to Evista
When Evista isn’t a perfect match, doctors turn to other drug classes. Below are the most frequently prescribed options.
Bisphosphonates
Alendronate is an oral bisphosphonate taken weekly to prevent spine and hip fractures. Other oral bisphosphonates include risedronate and ibandronate. Intravenous bisphosphonates such as Zoledronic acid are given once a year.
- Strong evidence for reducing both vertebral and hip fractures.
- Can cause esophageal irritation (oral forms) or acute‑phase flu‑like symptoms (IV).
- Not ideal for patients with severe kidney disease (eGFR < 30ml/min).
Denosumab
Denosumab is a monoclonal antibody given subcutaneously every six months that blocks bone‑resorbing cells. It works for patients who can’t tolerate oral bisphosphonates.
- Reduces both spine and hip fractures by roughly 40‑50%.
- Main concerns: rebound bone loss if injections stop, and rare cases of jaw osteonecrosis.
- Safe for people with moderate kidney impairment.
Hormone Replacement Therapy (HRT)
Estrogen‑based HRT (combined with progestin for women with a uterus) can protect bone, but it’s usually reserved for women who need relief from menopausal symptoms as well.
- Effective for spine and hip, but raises risk of breast cancer, blood clots, and stroke.
- Usually prescribed for the shortest time needed.
Calcitonin and Other Options
Salmon calcitonin nasal spray and oral forms offer modest vertebral‑fracture protection but are rarely first‑line because of limited efficacy.
Decision Criteria: How to Pick the Right Drug
Think of the choice as a checklist. Each factor pushes the balance toward one drug or another.
- Fracture risk profile - high hip‑fracture risk favors bisphosphonates or denosumab.
- Kidney function - eGFR < 30ml/min steers away from oral bisphosphonates; denosumab is safer.
- Gastro‑intestinal tolerance - difficulty swallowing pills or GERD points to IV bisphosphonate or denosumab.
- Frequency preference - daily Evista, weekly alendronate, monthly ibandronate, yearly zoledronic acid, or bi‑annual denosumab.
- Risk of blood clots - avoid Evista and HRT in patients with past DVT or pulmonary embolism.
- Cost and insurance coverage - generic alendronate is cheapest; denosumab and zoledronic acid are pricier.
Side‑Effect Snapshot
Below is a quick visual comparison of the most common adverse events for each drug class.
| Drug | GI Issues | Thrombo‑embolic Risk | Bone‑related Concerns | Other Notable Effects |
|---|---|---|---|---|
| Evista (Raloxifene) | Minimal | ↑ DVT/PE | None on hip | Hot flashes, leg cramps |
| Alendronate (oral bisphosphate) | Esophagitis, gastritis | Rare | Osteonecrosis (rare), atypical femur fracture (rare) | Acute‑phase flu‑like symptoms (first dose) |
| Zoledronic acid (IV bisphosphate) | None (IV) | Rare | Same as oral bisphosphonates | Flu‑like reaction, transient kidney rise |
| Denosumab | None | Low | Rebound loss if stopped, jaw osteonecrosis (rare) | Hypocalcemia risk, needs calcium/vit D |
| HRT (estrogen‑progestin) | Minimal | ↑ DVT/PE, ↑ stroke | Increased breast‑cancer risk | Hot flashes relief, mood changes |
Full Comparison Table
| Medication | Class | Administration | Dosing Frequency | Fracture‑Risk Reduction (Spine / Hip) | Main Side Effects | Typical Yearly Cost (AU$) | Best For |
|---|---|---|---|---|---|---|---|
| Evista (Raloxifene) | SERM | Oral tablet | Daily | 30‑40% / 0‑5% | Hot flashes, leg cramps, ↑ DVT | ≈ 350 | Women with high vertebral‑fracture risk who cannot tolerate bisphosphonates |
| Alendronate | Bisphosphonate | Oral tablet | Weekly | 45‑50% / 20‑25% | Esophagitis, flu‑like symptoms | ≈ 120 | First‑line for most post‑menopausal women |
| Zoledronic acid | Bisphosphonate (IV) | IV infusion | Yearly | 50‑55% / 30‑35% | Acute‑phase reaction, transient renal rise | ≈ 800 | Patients with GI intolerance to oral meds |
| Denosumab | RANKL inhibitor | Subcutaneous injection | Every 6 months | 45‑50% / 40‑45% | Hypocalcemia, rare jaw osteonecrosis | ≈ 1,400 | Renal‑impaired or bisphosphonate‑intolerant patients |
| Hormone Replacement Therapy | Estrogen‑Progestin | Oral or transdermal | Daily | 30‑35% / 20‑25% | ↑ breast‑cancer, ↑ clot risk | ≈ 600 | Women needing both bone protection & menopausal symptom relief |
Patient Scenarios - Which Drug Fits Best?
- Case A - 68y/o, mild kidney disease (eGFR45), hates pills. Denosumab avoids oral route and works with reduced renal function.
- Case B - 55y/o, recent DVT. Evista is contraindicated; an oral bisphosphonate like alendronate (if GI tolerated) or IV zoledronic acid would be safer.
- Case C - 72y/o, severe esophageal reflux. IV zoledronic acid or denosumab bypasses the esophagus.
- Case D - 60y/o, hot flashes bothering her. Evista may worsen hot flashes; HRT could actually help, but must weigh cancer risk.
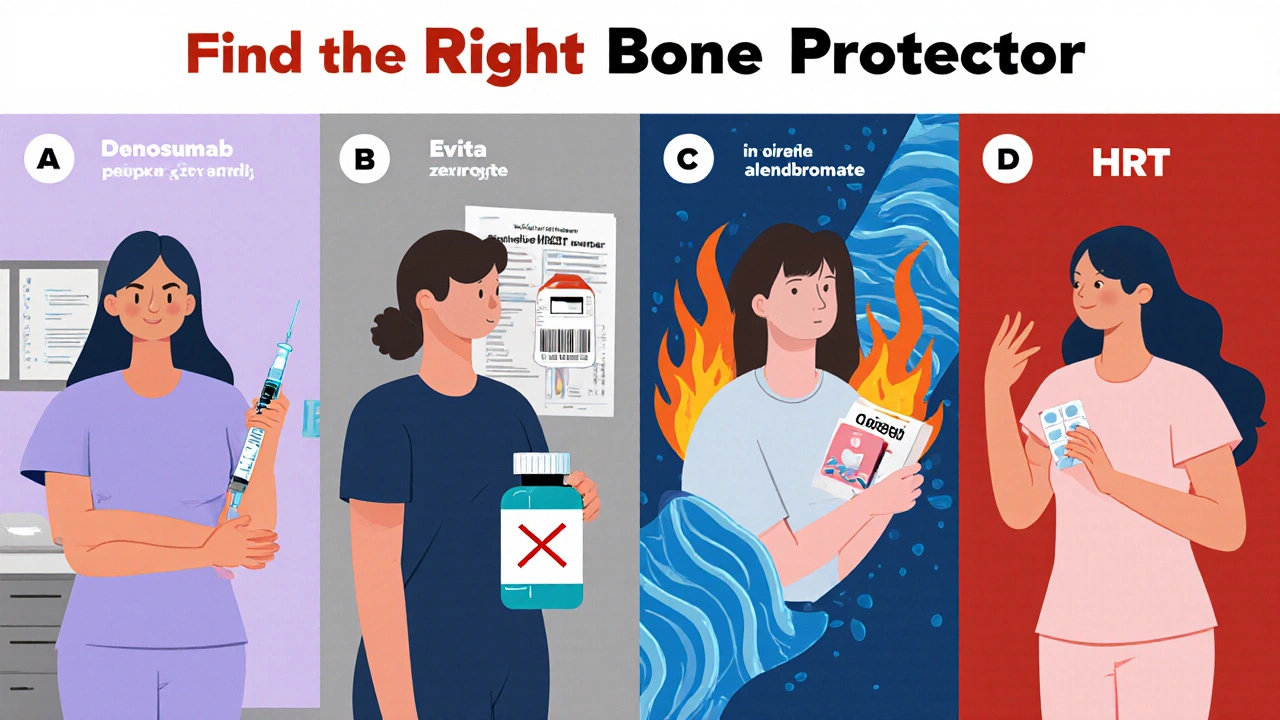
How to Decide - Quick Decision Tree
- Do you have a history of blood clots?
- Yes → Avoid Evista and HRT.
- No → Continue.
- Is your eGFR < 30ml/min?
- Yes → Pick denosumab (or IV bisphosphonate with caution).
- No → Continue.
- Can you swallow pills without irritation?
- No → Choose IV zoledronic acid or denosumab.
- Yes → Oral bisphosphonate (first‑line) or Evista if vertebral risk only.
- Do you need daily symptom relief (e.g., hot flashes)?
- Yes → Consider HRT if cancer risk acceptable.
- Cost concerns?
- Generic alendronate is cheapest; denosumab and zoledronic acid are higher‑priced options.
Checklist for Clinicians & Patients
- Confirm diagnosis (DXA T‑score≤‑2.5 or high‑risk FRAX).
- Assess kidney function (eGFR).
- Screen for prior clotting events.
- Discuss dosing convenience preferences.
- Review insurance coverage and out‑of‑pocket costs.
- Ensure adequate calcium (≥1,200mg) and vitaminD (≥800IU) intake before starting any bone‑active drug.
Frequently Asked Questions
Can I switch from Evista to a bisphosphonate?
Yes. A short drug‑free washout (usually 2‑4 weeks) is recommended before starting a bisphosphonate to avoid overlapping side‑effects. Your doctor will check calcium and vitaminD levels first.
Why doesn’t Evista protect the hip?
The SERM effect of raloxifene is strongest in trabecular bone (spine). Hip bone is more cortical, where raloxifene’s action is weaker, so studies haven’t shown a consistent hip‑fracture benefit.
Is denosumab safe for a 5‑year treatment plan?
Denosumab can be used long term, but you must continue injections without gaps. Stopping suddenly can cause rapid bone loss, so any discontinuation should be followed by another anti‑resorptive (often a bisphosphonate).
How does cost differ between oral and IV options?
Generic oral alendronate is the cheapest (≈AU$120 per year). IV zoledronic acid and denosumab are billed as specialist infusions or injections, typically ranging from AU$800‑1,400 per year, depending on coverage.
Should I take calcium supplements while on Evista?
Yes. Adequate calcium (1,200mg) and vitaminD are essential for any osteoporosis medicine, including Evista, to maximize bone‑building effect.
Next Steps
Armed with this side‑by‑side view, the next move is simple: schedule a visit with your healthcare provider, bring a copy of this guide, and discuss your personal risk factors, lifestyle preferences, and budget. Together you can pick the drug that keeps your bones strong and fits your life.
Comments
Tom Green October 17, 2025 at 13:28
Hey folks, great rundown here! If you’re weighing the pros and cons, think about how each medication fits into daily life – you don’t want a treatment that feels like a chore. For example, Evista’s daily tablet can be convenient for some, but weekly bisphosphonates might be better if you prefer fewer pills. Also, keep an eye on your kidney function when choosing a bisphosphonate; it’s a key safety check. Lastly, talk to your provider about calcium and vitamin D – they’re the foundation for any osteoporosis therapy.
Emily Rankin October 18, 2025 at 17:15
Reading this felt like watching a grand drama of bone health unfold on stage! The way Evista dances with estrogen receptors to protect the spine is almost poetic, yet the hip remains an elusive partner. Imagine the relief of a woman who can finally sleep through night sweats because she’s on HRT instead of battling hot flashes on Evista – that’s a narrative twist! In the end, the starring role belongs to the patient’s unique story, and we, as the audience, get to cheer for the best‑fit hero.
Rebecca Mitchell October 19, 2025 at 21:18
Evista works on spine not hip DVT risk is real but manageable
Lauren Sproule October 21, 2025 at 01:22
i think this guide is super helpful i love how it breaks down each drug into bite size pieces its like a spoonful of sugar for the brain lol, dont forget to check your insurance coverage before you pick a med because cost can be a real game changer
CHIRAG AGARWAL October 22, 2025 at 05:25
yeah this whole thing is kinda overhyped yo evista is just another pill you pop and hope for the best but if you can’t tolerate bisphos you might as well just go for the injection thing i don’t see the point of daily tablets if you’re scared of side effects
genevieve gaudet October 23, 2025 at 09:28
From a cultural perspective, it’s fascinating how different societies prioritize bone health – some rely heavily on diet, others on pharmacology. Evista, with its estrogen‑modulating effects, reflects a western approach to mimicking natural hormones, while in certain Eastern traditions, herbal remedies are still the first line. Either way, patient education remains the cornerstone of any regimen.
Patricia Echegaray October 24, 2025 at 13:32
Let’s not forget that the pharma giants are pulling strings behind the scenes, pushing Evista as a “safe” alternative while ignoring the hidden agenda. The true patriots know that natural bone strength comes from hard work, not a cheap chemical cocktail. If you care about your country’s future, demand transparency and steer clear of these corporate puppets.
Miriam Rahel October 25, 2025 at 17:35
In reviewing the comparative data, it is evident that bisphosphonates retain a superior efficacy profile regarding both vertebral and femoral fracture mitigation. While Evista demonstrates modest vertebral benefit, its inability to confer hip protection renders it suboptimal as a monotherapy in high‑risk cohorts. Moreover, the economic implications cannot be dismissed; generic alendronate presents a fiscally prudent option.
Samantha Oldrid October 26, 2025 at 20:38
Oh great another “miracle pill” – because we definitely needed more hype.
lisa howard October 28, 2025 at 00:42
The saga of osteoporosis treatment reads like an epic saga, each drug a character with virtues and tragic flaws. Evista, the reluctant hero, steps onto the stage with a noble aim to protect the spine, yet falters when the hip calls for aid. Bisphosphonates, the seasoned warriors, charge forward with both spine and hip victories, but they bear the scars of esophageal battles and rare, eerie femur fractures that whisper of caution. Denosumab, the enigmatic sorcerer, appears in a biannual cloak, wielding RANKL‑binding magic that sweeps away bone loss, yet warns of a perilous rebound should its enchantment be broken-an abrupt cessation that could unleash a storm of rapid bone degradation as if the very foundation of the body rebels. Hormone Replacement Therapy, the charismatic yet controversial diplomat, offers harmony for both bone and menopausal symptoms, but its court is riddled with intrigue-risks of breast cancer, clots, and stroke that loom like shadows over the realm. The cost, ever the ever‑present dragon, looms large; while generic alendronate slashes through the financial haze, denosumab and zoledronic acid roar with price tags demanding tribute. In the end, the physician‑patient pact must be forged with wisdom, taking into account personal histories of clotting, kidney function, gastrointestinal tolerance, and the simple desire for convenience-whether one prefers a daily tablet, a weekly dose, a yearly infusion, or a semi‑annual injection. The true victor is not a single drug, but the tailored symphony of choices that respects the individual’s unique health tapestry.
Cindy Thomas October 29, 2025 at 04:45
Interesting guide, but let me play devil’s advocate – what about those rare cases where patients actually do fine on lifestyle changes alone? 😊 Also, while most agree on calcium and vitamin D, the optimal dosing is still debated, so don’t take every number as gospel. That said, all the data you’ve compiled is solid, and I appreciate the balanced tone. Keep it up! 😄
Valerie Vanderghote October 30, 2025 at 08:48
Look, I get the whole “pick the right drug” spiel, but the emotional toll of being on medication 24/7 is huge. You’re not just swallowing pills; you’re constantly reminded of your fragility. The table’s numbers are cold, but real people feel anxious every time they think about a DVT risk or a possible jaw osteonecrosis. It’s like living with a shadow that might bite you when you least expect it. So, while the clinical efficacy is important, never underestimate the psychic burden – I’ve seen patients quit a perfectly good therapy because the fear was just too much. The healthcare team should address that fear head‑on, perhaps with counseling or support groups. Otherwise, we’re just prescribing fear in a pill form.
Michael Dalrymple October 31, 2025 at 12:52
Friends, let us take a moment to reflect on the complexity of osteoporosis management. In the realm of bone health, the clinician must weigh a plethora of variables: fracture risk, renal function, gastrointestinal tolerance, and even patient preference for dosing frequency. Evista, a selective estrogen receptor modulator, offers modest vertebral protection but falls short on hip fracture reduction; it also bears the consideration of increased thromboembolic risk. Bisphosphonates, particularly alendronate, demonstrate robust efficacy for both spine and hip but demand strict adherence to administration guidelines to mitigate esophageal irritation and rare atypical femoral fractures. Intravenous options such as zoledronic acid provide the convenience of an annual infusion, yet elicit transient flu‑like reactions and require careful renal monitoring.
Denosumab, administered subcutaneously every six months, has emerged as a potent alternative for patients intolerant to oral regimens, furnished with compelling reductions in vertebral and hip fractures. However, clinicians must remain vigilant regarding the phenomenon of rebound bone loss upon cessation, necessitating a well‑planned transition strategy, often to a bisphosphonate, to preserve gains.
Hormone replacement therapy remains a double‑edged sword: while it confers bone protection and relief from menopausal vasomotor symptoms, it amplifies the specter of breast cancer, cardiovascular events, and thromboembolic complications. Consequently, its indication is typically reserved for women who derive concurrent symptomatic benefit.
The economic landscape cannot be ignored. Generic alendronate, at an approximate annual cost of AU$120, stands as the most economical choice, whereas denosumab and zoledronic acid traverse the higher end of the pricing spectrum, imposing a financial consideration for many patients.
In sum, the judicious selection of an osteoporosis therapeutic agent demands a personalized, holistic approach. The clinician must synthesize clinical evidence with patient‑centred factors, fostering shared decision‑making, and ensuring that calcium and vitamin D adequacy underpin any pharmacologic regimen. Let us strive to empower our patients with knowledge and compassionate guidance, for the strength of bone is matched only by the strength of informed choice.
Emily (Emma) Majerus November 1, 2025 at 16:55
Great summary – remember calcium and vit D are key and talk to your doc about the best fit.