Chronic acid reflux isn’t just a nuisance-it’s a silent warning sign that could lead to cancer. If you’ve had heartburn for five years or more, especially if you’re a man over 50, overweight, or a smoker, you’re not just dealing with discomfort. You’re at risk for a type of cancer that’s rising fast and often caught too late.
What’s Really Happening in Your Esophagus?
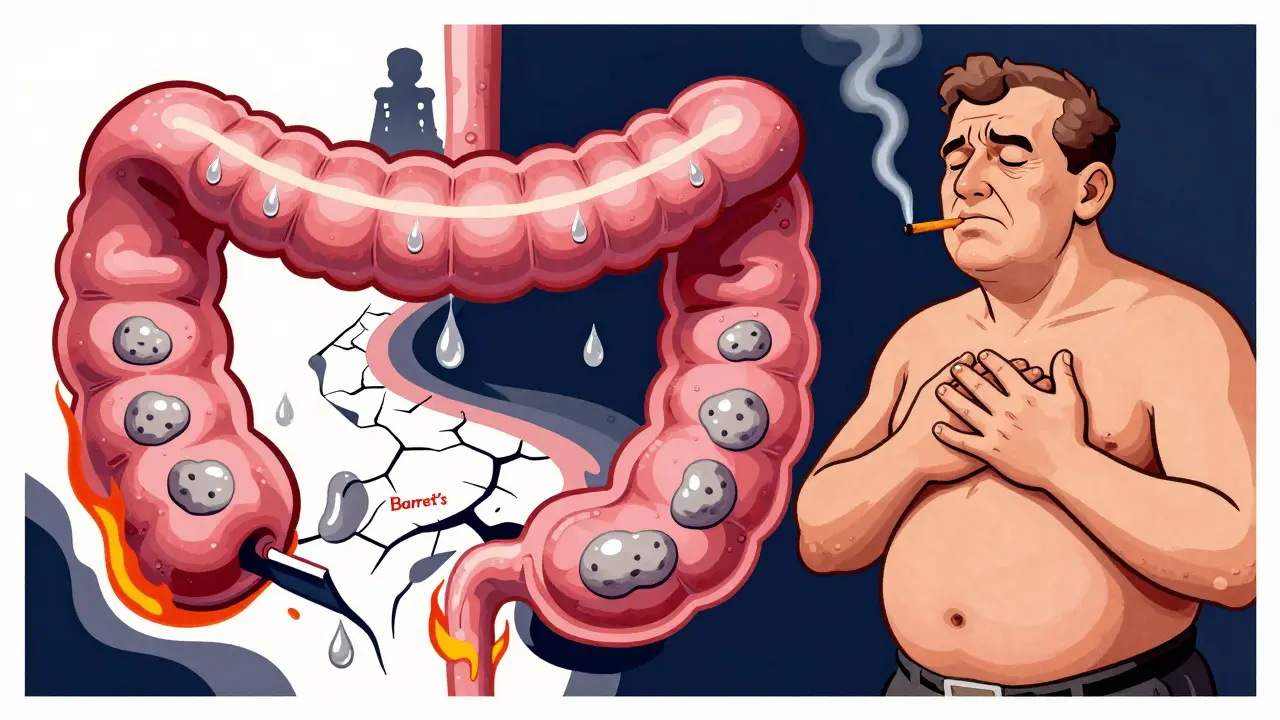
Every time stomach acid backs up into your esophagus, it’s like pouring vinegar on raw skin. Your esophagus isn’t designed to handle this. Over time, the constant burning triggers a survival response: the lining starts changing. Instead of normal squamous cells, it begins to look like stomach tissue. This is called Barrett’s esophagus. It’s not cancer yet-but it’s the only known precursor to esophageal adenocarcinoma, the most common type of esophageal cancer linked to GERD.
According to a 2023 NIH study, people with long-term GERD have a 3.2 times higher risk of developing esophageal cancer than those without it. That’s not a small increase. And the longer you have it, the worse it gets. If you’re having symptoms weekly, your risk jumps to 7 times higher. Most people don’t realize this isn’t about occasional heartburn after spicy food. It’s about years of daily or near-daily reflux-even if you’re on medication.
Who’s Actually at Risk?
Not everyone with GERD gets Barrett’s esophagus. Only about 10-15% do. But certain factors stack the deck. The biggest ones are:
- Being male (men are 3-4 times more likely than women)
- Age over 50 (90% of cases happen after 55)
- White, non-Hispanic ethnicity (risk is triple that of Black Americans)
- Obesity (BMI 30 or higher increases risk 2-3 times)
- Smoking (current or past, doubles or triples risk)
- Family history of esophageal cancer
Here’s the kicker: if you’re a white man over 50 with GERD for 10+ years, even if it’s mild, your risk of Barrett’s esophagus is significant. And if you add two or more of those other factors-like smoking and obesity-you’re in the high-risk zone. The American College of Gastroenterology says if you fit that profile, you should get an endoscopy. Yet only 13% of people who qualify actually do.
Red Flags That Mean You Need to See a Doctor Now
Most esophageal cancers are found at stage 3 or 4 because symptoms are ignored or mistaken for worsening GERD. But there are specific warning signs that shouldn’t be brushed off:
- Dysphagia-feeling like food gets stuck in your chest or throat. This shows up in 80% of diagnosed cases. It usually starts with solids, then moves to liquids.
- Unexplained weight loss-losing more than 10 pounds in six months without trying. This happens in 60-70% of cases.
- Chronic hoarseness or cough-lasting more than two weeks. Acid irritating your vocal cords can mimic a cold or allergies.
- Food impaction-food actually getting stuck and needing to be coughed out or swallowed with water repeatedly.
- Heartburn that’s getting worse-especially if you’re over 50 and it’s happening more than twice a week for five or more years.
These aren’t vague complaints. They’re measurable red flags. If you’ve had GERD for years and now you’re having trouble swallowing or losing weight, don’t wait. Delaying evaluation means missing the window for early treatment.

What Happens If You’re Diagnosed With Barrett’s Esophagus?
Barrett’s esophagus doesn’t mean you have cancer. But it does mean you need monitoring. The goal is to catch any precancerous changes-called dysplasia-before they turn into cancer.
Endoscopic surveillance is the standard. Doctors use a thin, flexible scope with a camera to look at your esophagus and take tiny tissue samples. If no dysplasia is found, you’re usually screened every 3-5 years. If low-grade dysplasia shows up, you might be monitored every 6-12 months. High-grade dysplasia? That’s a strong signal to remove the abnormal tissue before cancer develops.
Here’s the good news: if you catch it early, survival rates jump from 21% to 50-60%. That’s because treatment at this stage is less invasive-often done during the same endoscopy using heat, freezing, or laser therapy to destroy the bad cells.
How to Lower Your Risk-For Real
You can’t undo years of reflux, but you can stop it from getting worse. And some changes make a measurable difference:
- Quit smoking-within 10 years of quitting, your cancer risk drops by half.
- Lose weight-losing just 5-10% of your body weight cuts GERD symptoms by 40%. That’s because belly fat pushes stomach contents upward.
- Limit alcohol-stick to one drink a day for women, two for men. Heavy drinking raises a different type of esophageal cancer, but it still adds risk.
- Take PPIs consistently-if you have Barrett’s esophagus, taking proton pump inhibitors like omeprazole daily for five or more years reduces cancer risk by 70%.
- Don’t lie down after eating-wait at least three hours. Elevate the head of your bed by 6-8 inches.
And here’s something surprising: treating GERD early can cut your risk of developing Barrett’s esophagus by 40-60%. That’s not a guess-it’s from longitudinal studies. If you’ve had reflux for five years or more, getting on medication and sticking with it isn’t just about comfort. It’s prevention.

The Bigger Picture: Why This Is Getting Worse
Since 1975, esophageal adenocarcinoma rates have gone up by 850%. That’s not because of better detection. It’s because obesity and GERD have exploded. In 1980, 15% of U.S. adults were obese. Today, it’s 42%. More belly fat = more pressure on the stomach = more acid reflux.
And while squamous cell carcinoma (linked to smoking and alcohol) is declining, adenocarcinoma keeps climbing. The problem isn’t just medical-it’s societal. We’re eating more processed food, sitting more, and gaining weight. And we’re ignoring the signs until it’s too late.
The good news? We have tools to stop it. Endoscopic screening works. Weight loss works. Quitting smoking works. But only if you act.
What Should You Do Next?
If you have chronic GERD-especially if you’re a man over 50, overweight, or a smoker-ask your doctor about an endoscopy. Don’t wait for symptoms to get worse. Don’t assume your antacids are enough. The damage happens silently.
If you’ve already been diagnosed with Barrett’s esophagus, follow your screening schedule. Don’t skip appointments. Take your PPIs as prescribed. Track your weight. Quit smoking if you haven’t already.
And if you’re under 50 and have GERD? Start now. Change your habits. Lose weight if needed. Stop smoking. Eat earlier. Don’t lie down after meals. These aren’t just lifestyle tips-they’re cancer prevention.
Esophageal cancer is rare-but it’s deadly. And for people with long-term GERD, it’s not a matter of if, but when. The difference between life and death often comes down to one question: Did you get checked?
Can GERD cause esophageal cancer even if I’m on medication?
Yes. Medications like PPIs reduce acid and lower your risk, but they don’t eliminate it entirely. If you’ve had GERD for five or more years-even with medication-you’re still at risk for Barrett’s esophagus. That’s why long-term GERD, not just symptoms, is the key factor. Regular endoscopic screening is still needed if you’re in a high-risk group.
Is Barrett’s esophagus reversible?
In some cases, yes. With aggressive acid suppression (PPIs), weight loss, and quitting smoking, the abnormal lining can revert to normal in about 10-20% of patients. But it’s unpredictable. Even if it does improve, doctors still recommend ongoing monitoring because the risk doesn’t fully disappear.
Do I need an endoscopy if I have GERD but no symptoms?
Not if you’ve never had symptoms. But if you’ve had GERD for five or more years-even if your symptoms improved or disappeared-you should still be evaluated. Silent reflux can still cause damage. The American College of Gastroenterology recommends endoscopy for high-risk individuals (white men over 50 with chronic GERD plus two other risk factors), regardless of current symptom severity.
Can I get screened for Barrett’s esophagus without an endoscopy?
Not yet as a standard. Endoscopy is still the gold standard. But new tools are emerging. The Cytosponge-a pill-sized sponge on a string you swallow-is showing promise in trials. It collects cells from your esophagus and tests them for Barrett’s markers. One 2022 Lancet study found it detected 79.9% of cases. It’s not widely available yet, but it could change screening in the next few years.
How often should I get screened if I have Barrett’s esophagus?
It depends on what’s found. If no dysplasia is present, you’re usually screened every 3-5 years. If low-grade dysplasia is detected, you’ll need an endoscopy every 6-12 months. High-grade dysplasia often leads to treatment to remove the abnormal tissue. Always follow your gastroenterologist’s specific plan-don’t rely on general guidelines.
Does losing weight really help reduce my cancer risk?
Absolutely. Losing 5-10% of your body weight can cut GERD symptoms by 40%. That’s because belly fat increases pressure on your stomach, forcing acid upward. Less pressure means less reflux. Less reflux means less damage to your esophagus. Studies show weight loss reduces the progression from GERD to Barrett’s esophagus. It’s one of the most effective things you can do.
Why is esophageal cancer so deadly?
Because it’s usually found late. Early-stage esophageal cancer has no symptoms. By the time you feel trouble swallowing or lose weight, the cancer has often spread. The 5-year survival rate for all stages is only 21%. But if caught early-before it spreads-the survival rate jumps to 50-60%. That’s why screening high-risk people is critical. Early detection saves lives.
Comments
Joni O January 18, 2026 at 21:37
Just had my first endoscopy last month after 8 years of GERD-turns out I have low-grade dysplasia. Scared the hell out of me, but now I’m on PPIs, lost 12 pounds, and quit smoking. This post saved my life. Don’t wait like I did.
Robert Davis January 19, 2026 at 09:23
Look, I’ve been on PPIs for 12 years. I’m a 62-year-old white guy, overweight, smoked for 30 years. I’ve had heartburn since I was 35. And I still haven’t gotten the endoscopy. Why? Because my doctor says ‘you’re fine.’ But this article? It’s like he’s lying to me to avoid paperwork. I’m going next week.
Naomi Keyes January 19, 2026 at 10:50
While I appreciate the general tone of this post, it's worth noting that the NIH 2023 study referenced is actually a meta-analysis of 17 cohort studies, not a single prospective trial-and the 3.2x relative risk is only significant in those with persistent nocturnal reflux, which the article omits. Also, the 70% risk reduction with long-term PPI use? That's from a 2018 Gut paper with a 5-year follow-up, not 10. Please cite properly.
Eric Gebeke January 20, 2026 at 16:10
Of course they’re pushing endoscopies. Big Pharma makes billions off PPIs. You think they want you to lose weight and quit smoking? No-they want you to take pills forever. And don’t get me started on how the AMA is in bed with the GI industry. You think Barrett’s is real? Or is it just a money machine? I’ve been symptom-free for 4 years on diet alone. Why am I being pressured into a scope?
Max Sinclair January 21, 2026 at 05:47
Just wanted to say thank you for writing this. My dad passed from esophageal cancer last year-he ignored his reflux for 15 years because ‘it’s just heartburn.’ I’m 38, had GERD since 25, and got screened last month. No dysplasia. But I’m losing weight, sleeping upright, and I’ve never felt better. This isn’t fear-mongering. It’s fact-based care.
Praseetha Pn January 22, 2026 at 21:48
Wait-so you’re telling me the government and Big Pharma are using GERD to push endoscopies so they can sell cancer treatments? And they’re hiding the truth about how 5G towers and fluoridated water make acid reflux worse? I’ve been tracking my symptoms since 2019 and I’m 100% sure it’s the aluminum in my toothpaste. Also, my cousin’s neighbor’s dog got diagnosed with Barrett’s after eating a bag of chips. Coincidence? I think not.
Nishant Sonuley January 23, 2026 at 15:37
Look, I get it-GERD is a silent killer, but let’s not turn every guy with a burp into a walking cancer patient. I’m 52, overweight, had reflux since my 30s, and I’ve never had a single symptom beyond occasional heartburn after tacos. I eat clean, walk 8K steps a day, and I’m not getting scoped just because I’m a white guy with a beer belly. There’s a difference between being cautious and being paranoid. Also, I’m pretty sure the 850% increase since 1975 is just because we started calling every burp ‘Barrett’s’ in the 2000s.
Emma ######### January 24, 2026 at 10:07
My mom was diagnosed with high-grade dysplasia at 61. She didn’t have symptoms for years. Just lost 15 pounds and thought it was ‘getting old.’ They removed it with an endoscopy. She’s fine now. I’m 34 and got screened last year because of her. I don’t have Barrett’s-but I’m on PPIs, lost weight, and I don’t lie down after dinner anymore. It’s not about fear. It’s about respect-for your body, for your family.
Andrew Short January 25, 2026 at 01:13
You people are pathetic. You read one article and suddenly you’re all running to get scopes like it’s a cult initiation. I’ve had GERD for 20 years. I take a pill. I eat what I want. I don’t care if I live to 70 or 80. But I sure as hell don’t need some internet guru telling me I’m a ticking time bomb because I’m a man over 50. You’re not saving lives-you’re selling anxiety.
christian Espinola January 26, 2026 at 08:28
Let’s be real: if you’re a smoker, overweight, and on PPIs, you’re not preventing cancer-you’re just delaying the inevitable. The real cause? Glyphosate in your bread, soybean oil in everything, and corporate food poisoning. Endoscopies won’t fix that. Only a keto paleo vegan raw diet with Himalayan salt and cold showers will. And even then, the FDA is probably hiding the cure.
Ryan Otto January 27, 2026 at 04:00
While the epidemiological data presented is statistically significant, it is critically flawed in its causal inference. The correlation between obesity and esophageal adenocarcinoma is confounded by socioeconomic status, dietary patterns, and access to healthcare. Furthermore, the assertion that PPIs reduce cancer risk by 70% is derived from observational studies with significant recall bias. One must also consider that long-term PPI use is associated with increased risk of C. diff infection, hypomagnesemia, and bone fractures. The article’s tone is alarmist, and its recommendations lack nuance. In a properly regulated clinical environment, screening would be stratified by biomarkers-not demographics.