Biologic drugs aren’t like the pills you pick up at the pharmacy. You can’t just swap one brand for another and expect the same result. That’s because biologic drugs are made from living cells - not chemicals in a lab. And that changes everything.
What Makes Biologics So Different?
Think of a small-molecule drug - like aspirin or metformin - as a simple Lego block. It’s made of a few atoms arranged in a fixed pattern. You can recreate that exact structure over and over. That’s why generics exist. A generic version of a pill is chemically identical to the original. The FDA approves it without running new clinical trials because it’s the same molecule. Biologics are more like a living sculpture. They’re huge, complex proteins - often 1,000 times larger than small-molecule drugs. Humira, for example, is a monoclonal antibody made inside living Chinese hamster ovary cells. These cells are genetically engineered to produce the exact protein needed to treat rheumatoid arthritis. But even with perfect conditions, no two batches are exactly alike. Tiny differences in how the cells grow, how nutrients flow, or how temperature shifts by half a degree can change the final product. These aren’t errors. They’re normal. The FDA says it outright: “Slight modifications, or inherent variations, to the protein are expected as a natural process of manufacturing.” That’s not a flaw. It’s biology.How Are Biologics Actually Made?
Making a biologic isn’t mixing powders. It’s farming proteins. Here’s how it works:- Cell line development: Scientists tweak a cell’s DNA so it becomes a protein factory. This takes months.
- Upstream processing: The cells are grown in giant bioreactors - think 5,000 to 20,000 liters of nutrient-rich broth. Temperature, pH, oxygen, and food supply must be perfect. If the cells get stressed, they stop making the right protein. This phase lasts 10 to 14 days.
- Downstream processing: The protein is pulled out of the cell soup. It goes through multiple purification steps: protein A chromatography, viral filtration, ultrafiltration. Each step removes impurities. Even then, purity is 95-98%, not 100%.
- Formulation and packaging: The final product is mixed with buffers to stay stable. It’s then filled into vials or pens. Every step is monitored. One missed check can mean a $500,000 batch is scrapped.
Why Can’t You Make an Exact Copy?
You can’t copy a biologic the way you copy a pill because you don’t just copy the molecule - you copy the entire living system that made it. Even if another company gets the exact DNA sequence, they’re still using different cells. Different bioreactors. Different water sources. Different suppliers for raw materials. Different engineers running the process. All of these tiny differences add up. The final protein might look almost the same under a microscope, but its shape, folding, sugar attachments, or impurity profile could be subtly different. And those differences? They can affect how the drug works in your body. That’s why the FDA doesn’t approve “generic biologics.” Instead, they approve biosimilars. A biosimilar isn’t identical. It’s highly similar. And to prove it, the maker has to run dozens of analytical tests, animal studies, and even clinical trials to show it works just as well and is just as safe. One expert put it this way: “The manufacturing process itself becomes part of the product definition.” You can’t separate the drug from how it was made.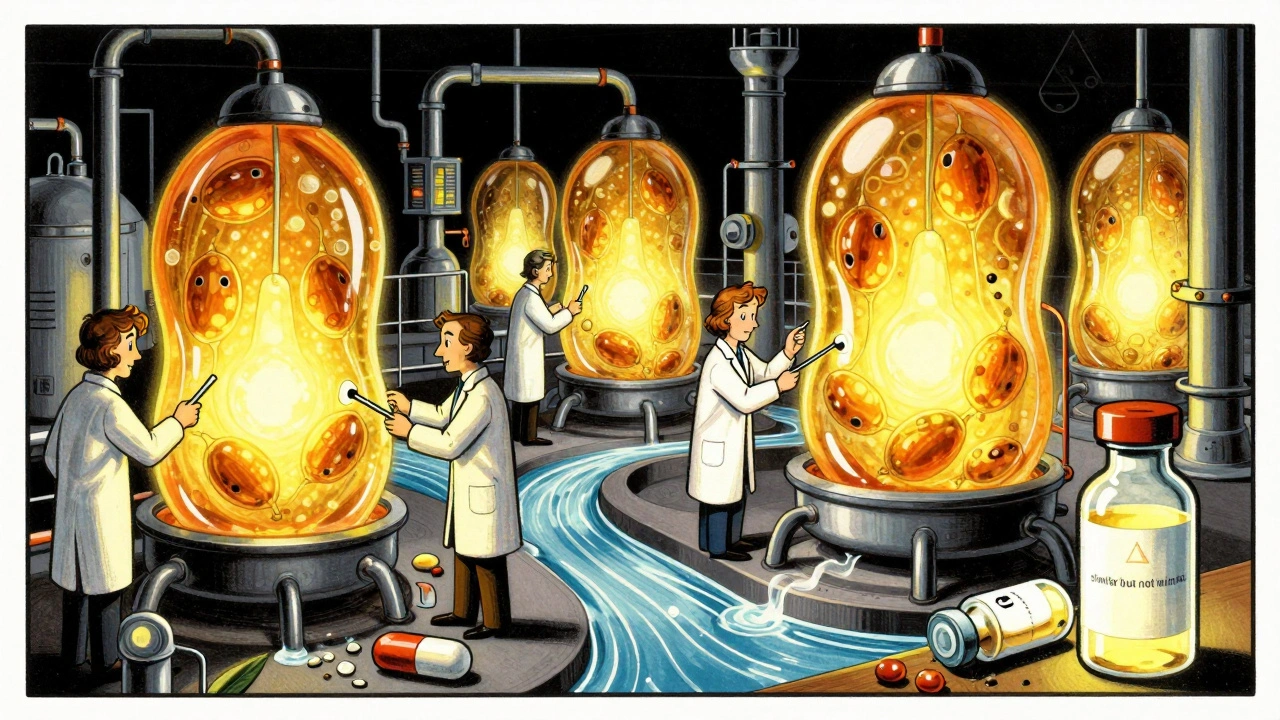
Biosimilars vs. Generics: The Real Difference
Here’s how they stack up:| Feature | Generics | Biosimilars |
|---|---|---|
| Drug Type | Small molecule (chemical) | Large molecule (biological) |
| Size | 500-1,000 Daltons | 150,000+ Daltons |
| Manufacturing | Chemical synthesis | Living cell cultures |
| Identical to Original? | Yes - chemically identical | No - highly similar, not identical |
| Approval Pathway | Abbreviated (no new clinical trials) | Extensive analytical, non-clinical, and clinical data required |
| Typical Cost Reduction | 80-90% | 15-35% |
Why This Matters for Patients
If you’re on Humira, Enbrel, or Ozempic, you might hear about a cheaper version coming. But don’t assume it’s a drop-in replacement. Your doctor needs to know it’s a biosimilar - not a generic. Some states require pharmacists to notify you before switching. Insurance companies might push for biosimilars to save money. But the science says: you can’t just swap them like you would two brands of ibuprofen. There’s also a psychological factor. Patients on biologics often have chronic, serious conditions. They’ve built trust with their current treatment. Switching to something “similar but not the same” can cause anxiety. That’s why many doctors prefer to keep patients on the original unless there’s a clear, documented benefit.
The Future: Can We Ever Make Exact Copies?
Right now, the answer is no. And experts don’t think that will change. Even with AI, real-time sensors, and single-use bioreactors, we still can’t fully map every single variation in a biologic. Dr. R. Lou Sherman from the Alliance for Advanced Biologics says: “Current analytical methods can characterize only 60-70% of a typical monoclonal antibody’s structural attributes.” That means we’re blind to 30-40% of what’s in the drug. The industry is moving toward more flexible, modular manufacturing. That could make biosimilars cheaper and faster to produce. But the core truth remains: living systems are messy. And that messiness is what makes biologics work - and what makes them impossible to copy exactly.What’s Next for Biologics?
The market is exploding. In 2023, biologics made up 42% of global drug sales. By 2028, that’s expected to hit 52%. New types are coming - bispecific antibodies, cell therapies, gene therapies. All of them are made the same way: with living cells. That means the demand for biosimilars will keep growing. But so will the need for better testing tools, smarter manufacturing, and clearer regulations. Right now, the FDA and EMA have over 200 and 300 pages of rules just for biologics manufacturing. And every batch? Thousands of pages of documentation. The challenge isn’t just science. It’s systems. It’s trust. It’s cost. And above all, it’s accepting that some things - especially living ones - can’t be perfectly replicated. And maybe that’s okay. Because in medicine, sometimes the complexity isn’t a bug. It’s the feature.Can biosimilars be substituted for biologics without a doctor’s approval?
In many places, pharmacists can’t automatically swap a biologic for a biosimilar without the prescriber’s permission. Rules vary by state and country. Some require the doctor to specifically write “dispense as written” or “no substitution.” Always check with your pharmacist or provider before switching.
Why are biosimilars so much cheaper than the original biologic, but not as cheap as generics?
Biosimilars still require massive investment: specialized facilities, trained staff, complex testing, and clinical trials to prove similarity. A generic pill can be made in a standard factory with off-the-shelf chemicals. A biosimilar needs a $500 million biologics plant. The savings come from avoiding the full cost of developing the original drug - not from cutting corners on production.
Are biosimilars safe?
Yes - but only if they’ve been approved. The FDA and EMA require biosimilars to show no meaningful differences in safety, purity, or potency compared to the original. Thousands of patients have used biosimilars for years with no new safety signals. But because they’re not identical, switching isn’t always automatic. Your doctor will monitor you closely if you change.
Can I tell if I’m on a biosimilar?
Yes. The packaging and prescription label will list the biosimilar’s name, which is different from the original. For example, a biosimilar to Humira might be called “Adalimumab-adbm.” Your pharmacy will also notify you if a switch is made. If you’re unsure, ask your pharmacist or check your prescription details.
Do biosimilars work as well as the original biologics?
Clinical trials show they do. In studies comparing biosimilars to their reference biologics, there’s no meaningful difference in how well they reduce inflammation, lower blood sugar, or shrink tumors. The FDA requires this proof before approval. Real-world data from Europe and the U.S. over the last decade supports this - patients respond the same way.
Why can’t we just use the same cell line as the original drug maker?
Even if you had the exact same cell line, the manufacturing environment would still differ - bioreactors, water quality, nutrient batches, even the air in the cleanroom. These small variations affect how the cells behave. That’s why regulators require each biosimilar to be tested as its own product, even if the DNA is identical.

Comments
Hamza Laassili December 13, 2025 at 19:55
This is why America needs to stop outsourcing biologics to China!! 🇺🇸 These living-cell factories? They should be HERE. We're letting foreign labs make our life-saving drugs and then wonder why prices are crazy. I don't care if it's 'biology'-we can build rockets to Mars but can't make a damn antibody right here?! #BuyAmerican #BiologicsAreNotToys
Casey Mellish December 14, 2025 at 12:54
Fascinating breakdown! As an Aussie who’s seen our healthcare system struggle with biologic access, I’ve got to say-this explains why our PBS (Pharmaceutical Benefits Scheme) takes forever to approve biosimilars. It’s not bureaucracy-it’s science. We need more public education like this. Kudos for making complex biology feel human. 🇦🇺✨
Emily Haworth December 14, 2025 at 23:59
Wait… so you’re telling me the government doesn’t know what’s REALLY in these drugs?? 😳 I knew it! They’re hiding something. 30-40% of the drug is UNCHARTED?! That’s not biology-that’s a cover-up. 🤫💉 Who’s controlling the bioreactors? Big Pharma? The Illuminati? 🌐👁️ #BiologicConspiracy
Tom Zerkoff December 15, 2025 at 03:52
Thank you for this meticulously detailed exposition. The distinction between generics and biosimilars is profoundly underappreciated in public discourse. The regulatory rigor applied to biosimilars-spanning analytical characterization, non-clinical assessment, and clinical equivalence trials-represents a paradigm of scientific integrity. One cannot reduce biological complexity to chemical equivalence without compromising patient safety.
Yatendra S December 15, 2025 at 04:45
You know… life is messy. That’s why God made biologics. 🤔 We try to control everything-machines, algorithms, pills-but biology? It breathes. It changes. It whispers in sugar chains and folded proteins. Maybe we’re not supposed to copy it. Maybe we’re supposed to respect it. 🌱 #DeepThoughts
Himmat Singh December 15, 2025 at 05:37
I must respectfully contest the premise. The assertion that biosimilars cannot be identical is a self-serving narrative propagated by originator manufacturers to maintain monopolistic pricing. If two molecules exhibit the same amino acid sequence, the claim of non-identicality is a semantic construct designed to justify price differentials. The science does not necessitate such distinction.
Tommy Watson December 15, 2025 at 18:21
So… we’re paying $20K a year for a drug that’s basically a fancy protein smoothie made by sad hamster cells?? 😭 I’m not mad… I’m just disappointed. Why can’t we just… clone the cells? Or like… 3D print the protein? This feels like a scam. #BiologicScam #IWantMyMoneyBack
Donna Hammond December 16, 2025 at 17:18
This is so important for patients with autoimmune diseases. I’ve been on Humira for 8 years. When my insurance switched me to a biosimilar, I was terrified. But my rheumatologist walked me through the data-same efficacy, same safety profile. I’m still doing great. If you’re nervous about switching? Talk to your doctor. You’re not alone. 💙
Willie Onst December 16, 2025 at 20:57
Man, this is wild. I always thought generics = exact copy. But biologics? They’re like trying to recreate your grandma’s soup recipe… but you don’t know what spices she used, and the pot’s different, and the stove’s on a different floor. 🍲 You get close. But it’s not the same. And honestly? That’s kind of beautiful.
nithin Kuntumadugu December 18, 2025 at 08:46
Let’s be real-this whole biosimilar thing is a corporate shell game. The ‘complexity’ is just a smokescreen to delay competition. Why does a $500M facility need to exist? Why can’t we standardize the cell lines? Because they want you to think it’s magic. It’s not. It’s profit. 💸 #BigPharmaLies
John Fred December 19, 2025 at 09:40
The upstream/downstream pipeline is a beast. I’ve seen bioreactors in action-99.9% purity is a win. The impurity profiles? They’re like fingerprints. That’s why the FDA requires so much data. It’s not red tape-it’s risk mitigation. 🔬💡 #BiopharmaLife
Harriet Wollaston December 20, 2025 at 14:47
I just want to say thank you for writing this. My sister has Crohn’s and was on a biologic for years. When her insurance switched her to a biosimilar, she cried. Not because she didn’t trust it… but because she was scared to lose the stability she’d fought so hard for. This isn’t just science. It’s someone’s peace of mind. ❤️