Nonmelanoma skin cancer is the most common cancer in humans - and most people don’t even realize it. Two types make up nearly all of these cases: basal cell carcinoma and squamous cell carcinoma. They’re not the same. One grows slowly and rarely spreads. The other can turn dangerous fast. Knowing the difference isn’t just about medical facts - it’s about catching it early enough to stop it before it causes real harm.
Where They Start: The Skin’s Layers
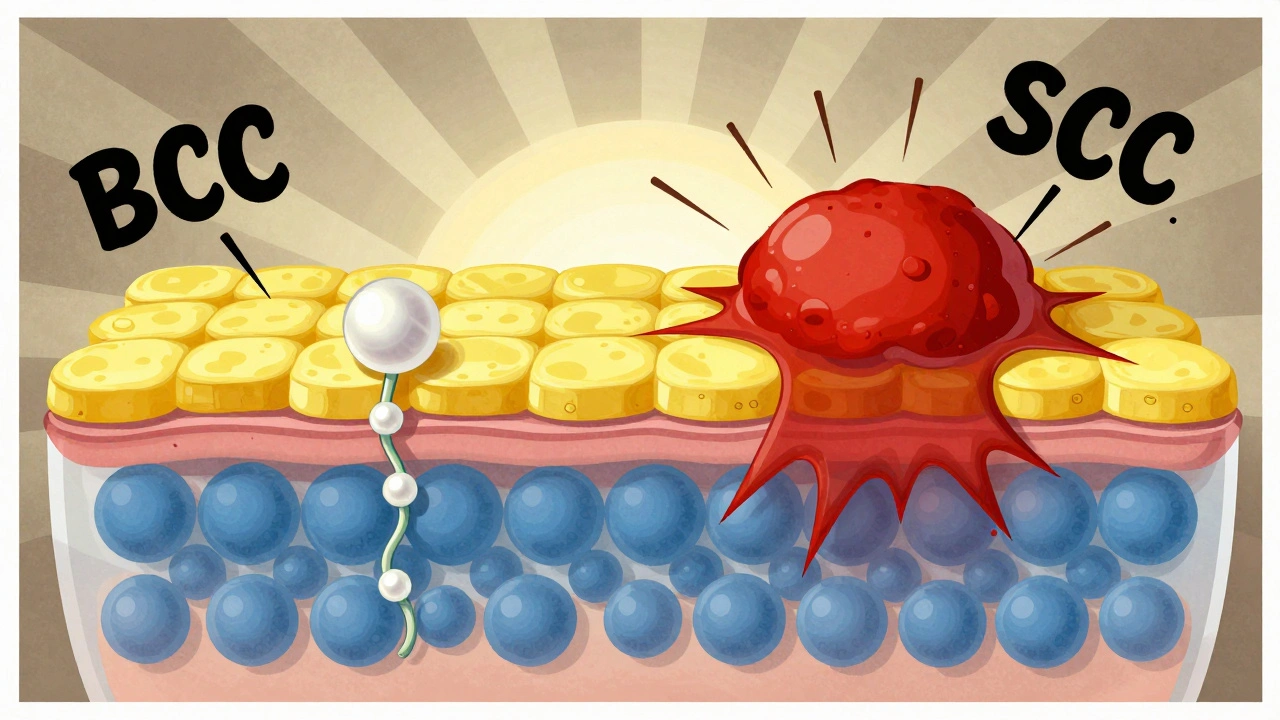
Your skin has layers. The top layer, the epidermis, is made of flat, scale-like cells called squamous cells. Below them, in the deepest part of the epidermis, are round basal cells. These basal cells keep dividing, pushing older cells upward. As they rise, they flatten out and become squamous cells. That’s how your skin renews itself every few weeks. Basal cell carcinoma starts in those bottom-layer basal cells. Squamous cell carcinoma starts in the upper squamous cells. That tiny difference in origin leads to big differences in how they behave.What They Look Like: Spotting the Signs
Basal cell carcinoma often shows up as a shiny, pearly bump - like a tiny pearl under the skin. It might look like a sore that won’t heal, or a scar-like patch that’s flat and waxy. These usually appear on the face, ears, or neck. About 70% of BCCs are pearly bumps. Another 20% are open sores that bleed or crust over and never fully close. Squamous cell carcinoma looks different. It’s often a firm, red bump, dome-shaped and raised. Sometimes it looks like a wart, or a scaly, red patch that won’t go away. These can also bleed or crust. About 45% of SCCs are dome-shaped growths. Another 20% are scaly patches. Unlike BCC, SCC often feels rough to the touch - like sandpaper. Both can look harmless at first. Many people ignore them, thinking it’s just a pimple or a dry patch. But if something on your skin doesn’t heal in 4-6 weeks, or keeps coming back after you’ve tried to treat it, get it checked.How Fast They Grow: Speed Matters
Basal cell carcinoma creeps along. On average, it grows about half a centimeter to one centimeter per year. It’s slow. So slow that people often wait months - sometimes years - before seeing a doctor. That’s why it’s so common. It doesn’t hurt. It doesn’t itch. It just sits there. Squamous cell carcinoma moves faster. It can grow 1.5 to 2 centimeters in a year. Some aggressive types double in size in just 4-6 weeks. That’s why SCC patients often report sudden changes - a spot that was small last month is now the size of a pea. The speed is a red flag.Who Gets It: Risk Factors
Both cancers are tied to sun exposure. But not the same kind. Basal cell carcinoma is linked to intense, occasional sunburns - like a bad day at the beach as a kid or teen. People with fair skin, blue eyes, and light hair are most at risk. Men get it slightly more often than women - 55% to 45%. Squamous cell carcinoma is tied to long-term, cumulative sun exposure. Think farmers, construction workers, lifeguards. It’s more common in people over 50. About 85% of cases occur in people older than 50. Men are more likely to get it - 65% of cases. That’s because of decades of sun exposure on the job. There’s another group at high risk: organ transplant recipients. Their immune systems are suppressed to prevent rejection. For them, the risk of SCC is 250 times higher than the general population. For BCC, it’s only 10 times higher. That tells you how much more dangerous SCC can be when the body can’t fight back.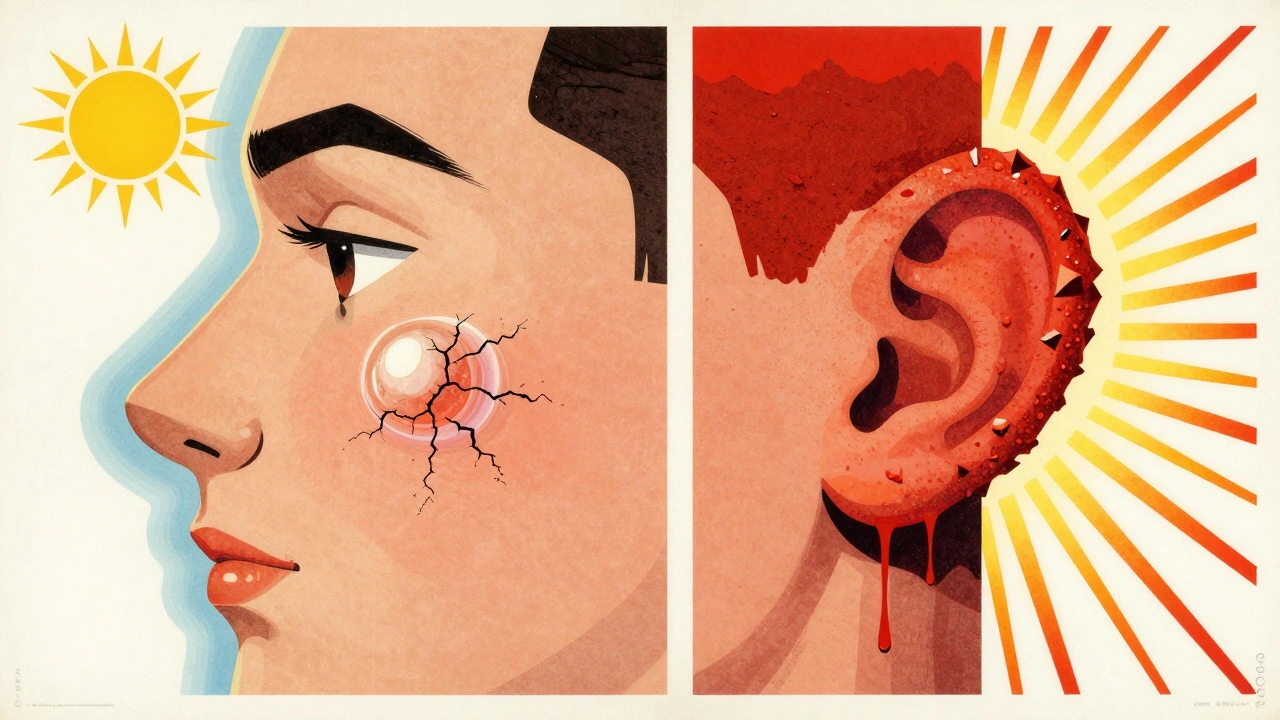
How Dangerous They Are: Metastasis Risk
Here’s the big difference: metastasis. Basal cell carcinoma almost never spreads. Fewer than 0.1% of cases become metastatic. Even if left untreated for years, it rarely moves beyond the skin. But that doesn’t mean it’s harmless. Left alone, it can destroy tissue - eating into cartilage, bone, or nerves. A BCC on the nose can grow deep enough to damage the eye socket. It’s ugly. It’s disfiguring. But it’s not usually deadly. Squamous cell carcinoma can spread. About 2-5% of cases metastasize. That’s 10 times more than BCC. If it spreads to lymph nodes or organs, survival drops sharply - from 95% to 25-45% over five years. High-risk areas? Lips, ears, and genitals. SCC on the lip has a 14% chance of spreading. On the ear, it’s 9%. That’s why doctors treat SCC on these spots more aggressively.Treatment: What Happens When You Go to the Doctor
Both cancers are highly treatable - if caught early. Surgical removal is the most common method. For BCC, doctors often use Mohs surgery, which removes the tumor layer by layer, checking each one under a microscope. It’s 99% effective for primary BCC. For SCC, Mohs surgery is still used, but cure rates are slightly lower - around 97%. Why? Because SCC tends to grow deeper and wider. That means doctors need to cut out bigger margins - 4 to 10 millimeters - compared to 3 to 5 for BCC. Topical creams like imiquimod or 5-fluorouracil work for some superficial BCCs - about 60-70% success. But they’re only 40-50% effective for SCC. That’s because SCC digs deeper. Creams can’t reach it. Patients with SCC need more follow-ups. On average, they have 2.3 times more visits than BCC patients. Why? Because SCC is more likely to come back. In immunocompromised people, recurrence rates for SCC are 15% - five times higher than for BCC.Recovery and Aftercare
BCC patients often need just one treatment. 92% are cured after one go. SCC patients? Only 78% are cured with one round. Many need repeat procedures. That’s why SCC patients report more anxiety - not just about the cancer, but about the process. Reconstructive surgery is more common with SCC. About 45% of SCC patients need skin grafts or flaps after removal, compared to 28% for BCC. That’s because SCC often requires deeper excision. Sun protection is critical for both. Daily sunscreen reduces BCC risk by 40%. For SCC? It cuts risk by 50%. That’s because SCC is more directly tied to years of sun damage, not just one bad burn.
Comments
David Palmer December 11, 2025 at 14:46
bro i had this thing on my nose for like 6 months thought it was a zit lol
Jimmy Kärnfeldt December 11, 2025 at 21:21
Really appreciate this breakdown. I used to think skin cancer was just about moles and melanoma. Learning that something as "harmless" as a pearly bump could be BCC is eye-opening. It’s wild how our skin quietly screams for attention. Glad we’re getting better at catching these early.
Also, the part about transplant patients being 250x more at risk for SCC? That’s terrifying but important. Makes me wonder how many cases go undiagnosed because people assume they’re just "old age spots."
Taylor Dressler December 12, 2025 at 10:19
Just want to add something practical: if you're over 40 and spend any time outdoors, get a baseline full-body skin map done by a derm. Take photos of every mole and bump. Compare them every 6 months with the same lighting. It’s the easiest way to catch changes before they become problems.
Also, sunscreen isn’t just for beach days. UV exposure accumulates even through windows and on cloudy days. That 50% risk reduction for SCC? That’s real. Don’t skip the SPF 30+ every morning.
And yes - if it doesn’t heal in 4 weeks, get it checked. No excuses.
Ariel Nichole December 13, 2025 at 03:00
Thank you for sharing this. I had a BCC removed last year and didn’t realize how common it was until I started reading up on it. The Mohs surgery was way less scary than I thought - they numbed it up and I just watched TV during it. Honestly, the hardest part was waiting for the results.
Now I wear a hat every day and reapply sunscreen like it’s my job. It’s weird to think something so small could’ve turned into something big if I’d ignored it.
Katherine Liu-Bevan December 13, 2025 at 23:01
One thing the article doesn’t mention enough: SCC on the lips is a silent killer. I lost my uncle to metastatic SCC that started as a "dry patch" on his lower lip. He thought it was chapped lips from smoking. By the time he went in, it had spread to his lymph nodes. He was 58.
Don’t let anyone tell you "it’s probably nothing." If it’s persistent, rough, bleeding, or changing - get it biopsied. Even if you’re healthy. Even if you’re young. Early detection saves lives. Period.
matthew dendle December 14, 2025 at 12:19
so like... if i got a pimple on my ear and it dont go away in 2 weeks its cancer? lol jk kinda
but seriously why do docs make it sound like every bump is gonna kill you? i had one on my neck for a year and it turned out to be a cyst. they still biopsied it tho. wasted my time and 300 bucks
Jean Claude de La Ronde December 15, 2025 at 23:29
It’s funny how we treat skin like it’s disposable. Like, "oh it’s just a bump," but your skin is your largest organ. It’s literally your body’s first line of defense.
And yet we tan like it’s a fashion statement. We skip sunscreen because "it’s cloudy." We ignore the weird spot because "I’m too busy."
Maybe the real cancer isn’t the cells - it’s the denial.
Ben Greening December 17, 2025 at 13:43
The data on SCC recurrence in immunocompromised patients is particularly sobering. In clinical practice, we see a stark contrast: BCC patients often come in for a single visit and then vanish. SCC patients return every 3–6 months for years. Their anxiety is palpable. It’s not just medical - it’s psychological. The fear of recurrence lingers.
And while AI-assisted diagnosis is promising, it’s not a replacement for clinical judgment. I’ve seen algorithms miss SCCs that looked like psoriasis. Human eyes still matter.
Mia Kingsley December 18, 2025 at 02:13
okay but why is everyone acting like this is new info?? i’ve been telling my family for YEARS that if you have a weird spot on your face just get it checked and they’re like "oh you’re dramatic" and then one of them got a SCC on their ear and now they’re crying in the car asking me if they’re gonna die
why do we wait until someone almost dies to listen to the person who’s been screaming into the void??
john damon December 18, 2025 at 11:52
my uncle got 2 BCCs and 1 SCC and now he’s like a walking sunscreen ad 🧴😎
he wears a hat indoors now. no joke. even in the mall. he says "better safe than sorry"
also he took a pic of his skin every month and made a whole google folder 😂
weird? yes. smart? absolutely.